7.5% Salaried professional discount
10% Young family discount (all are 40 years or below at first inception, and will continue for the lifetime of the policy, irrespective of claims.
No Entry Age Limit
Supercharge bonus; optional cover: Get bonus of 100% of sum insured every year, irrespective of claims; max up to 500% of base sum insured.
No CO- PAY with Room rent limit of Single Private a/c Room.
No Zone CO-Pay for Medicare Premier, Select, Top Up Plan
optional cover Must Have – Consumables Coverage, Preventive Health Checkup, Supercharge bonus
BP, Sugar – No loading for Fresh Business.
Policy Wordings
TATA AIG General Insurance Company Limited (We, Our or Us) will provide the insurance, described in this Policy and any endorsements thereto, for the Policy Period, as defined in the Policy to the Insured Person(s) named in the Policy Schedule based on the Disclosure to Information Norm, including in reliance upon the statements contained in the Proposal Form or any other mode of communication which shall be the basis of this Policy and are deemed to be incorporated herein in return for the receipt of the required premium in full and compliance with all the applicable terms, conditions and exclusions of this Policy. The insurance provided under this Policy is only in force for the Insured Person with respect to such and so many of the benefits as indicated in the Policy Schedule and up to the Sum Insured/limits set opposite such benefit(s).
The statements contained in the Proposal signed by the Policyholder (You) shall be the basis of this Policy and are deemed to be incorporated herein. The insurance cover is governed by and subject to, the terms, conditions and exclusions of this Policy.
Your Obligations
Please disclose all pre-existing disease/s or condition/s before buying a policy. Non-disclosure may result in claim not being paid and termination of Your policy.
ABCD, Surgeries, Treatment,
Regular Medication: Now a days single Tablets for combination of Diseases are prescribed, so if you hide some issues, it will be known at the time of Hospitalization, and claim will be rejected.
Preamble
While the policy is in force, if the Insured Person contracts any disease or suffers from any illness or sustains bodily injury through accident and if such event requires the insured Person to incur expenses for Medically Necessary Treatment, We will indemnify You for the amount of such Reasonable and Customary Charges or compensate to the extent agreed, upto the limits mentioned, subject to terms and conditions of the Policy. Each Benefit is subject to its Sum Insured, but Our liability in aggregate to make payment in respect of any and all Benefits shall be limited to the Sum Insured unless expressly stated to the contrary.
In case of family floater policy, the sum insured for all or any of the benefits shall be on a per policy per year basis unless explicitly stated to the contrary. In case of individual policy, the sum insured for all or any of the benefits shall be on per insured per year basis unless explicitly stated to the contrary.
The said Medically Necessary Treatment must be on the advice of a qualified Medical Practitioner.
PRODUCT HIGHLIGHTS
- Professional Discount FOR SALARIED CUSTOMERS, No Entry Age Limit -7.5%
- Young Family Discount FOR FAMILIES BELOW 40 YEARS – 10%
Suitability
| Entry Age: Minimum | Child– 0 days Dependent children between 0 days and 5 years can be insured only when both parents are getting insured. Adult– 18 years |
| Entry Age: Maximum | Child– 25 years Adult– No limit (Life Long eg: 100) |
| Cover Ceasing age | There is no maximum cover ceasing age under this policy. |
| Policy Term | 1 Year/ 2 Years/ 3 Years |
| Renewal | Life long renewal |
| Coverage Options | Individual/Family floater / Multi Individual (1 – 10) |
| Age of Proposer | 18 years or above |
| Relationships Covered | The family includes spouse, economically dependent children and parents/parents-in-law. Relationships covered: Self, spouse and up to 3 dependent children, up to 2 parents and up to 2 parent-in-laws. In case of family floater, where the dependent child(ren) attains 26 years of age at renewal, the child(ren) can be covered under a separate policy with eligible continuity benefit. The Multi-individual policy covers Self, Spouse/ Partners, Upto 3 Dependent Children, Parents & Parents-in-law, Grandparents, Grandchildren, Siblings (Sister/Brother), Uncle, Aunt, Nephew, Niece, Employee, Domestic Help and Legal Guardian. i.e SELF SPOUSE SON DAUGHTER FATHER MOTHER FATHER IN LAW MOTHER IN LAW SISTER BROTHER SISTER IN LAW BROTHER IN LAW GRAND SON GRAND DAUGHTER GRAND FATHER GRAND MOTHER |
| Discount | Long term Discount: 5% for a policy term of 2 years 7.5% for a policy term of 3 years Note: better go with Long Term of 3 years, so that your premium will be Locked, as based on the Claims, Every Insurance company will request IRDAI to increase their Premium in order to settle the claim and for their Survival, so, every company will increase premium up to 12% on Renewals, Instead of 5 years Slab. Professional Discount: 7.5% of discount (This discount is applicable for salaried customers), (PF No. is mandatory to avail this discount.) Young Family Discount: 10% of discount is applicable only if all the Insured Persons covered are of age of 40 years or below at the time of first inception of the policy. This discount will be effective from the first year of the policy and will continue for the lifetime of the policy, irrespective of claims. This discount will be discontinued if, at any point during the policy year, a new member is added whose entry age in policy is 40 years or above. Favorable Experience Discount: 20% at the inception of the policy. At Renewal, the Favorable Experience Discount may vary based on established criteria. Note: First Time Purchase is Zero Year and Renewal years will be First, Second and Third etc… |
| Claim Years in last 3 Policy Years | Favorable Experience Discount |
| 3 Years | 0% |
| 2 Years | 5% |
| 1 Year | 10% |
| No Claim | 20% |

Sum Insured options (in ₹) :
- 5 Lacs
- 7.5 Lacs
- 10 Lacs
- 15 Lacs
- 20 Lacs
- 25 Lacs
- 50 Lacs
- 75 Lacs
- 100 Lacs
- 200 Lacs
- 300 Lacs (3CR)
Zone(s)
For the purpose of premium computation, the country is divided into following three Zones and premium payable under this Policy will be computed based on the zone as applicable for the ‘Address’ of the proposer/ Insured Person:
| Zone A | Mumbai (including Mumbai Metropolitan Region), Delhi (including National Capital Region, Faridabad, Ghaziabad), Ahmedabad, Surat, Baroda and Hisar |
| Zone B | Hyderabad (including Secunderabad), Sangareddy, Bengaluru, Kolkata (including Kolkata Metropolitan Area, Howrah, Hoogly), Indore, Gwalior, Chennai, Chandigarh (including, Mohali, Punchkula, Zirakpur), Pune (including Pimpri Chinchwad), Rajkot, Gandhinagar, Patan, Mahesana, Sabarkantha, Banaskantha, Junagadh, Navsari, Kheda, Arvalli, Mahisagar, and Surendranagar |
| Zone C | Rest of India |
Here ‘Address’ implies the place where the person ordinarily resides. In case proposed prospect(s) reside at multiple addresses, then address of the person residing in the highest zone will be considered.
Lifelong renewal:
We offer you a lifelong renewal for your policy provided premium is paid without any break. Your premiums will be basis the age, sum insured, zone, optional cover(s) and applicable discounts, if any. Your renewal premium will be basis your age on renewal and applicable discounts, if any. There will be no extra loadings based on your individual claim.
The policy is renewable except in the case of established fraud or non-disclosure or misrepresentation by the Insured Person.
Pre-policy medical check-up:
Pre-Policy Check-up at our network may be required based upon the age and/or Sum Insured. The medical reports are valid for a period of 90 days from the date of Pre-Policy Checkup.
| Age(Yrs)/Sum Insured | Up to 50 Lacs | 75 Lacs & 100 Lacs | 200 Lacs & 300 Lacs |
| Upto age 45 | Tele/Video MER (only if positive medical declaration) | Tele/Video MER | |
| 46 – 55 | Tele/Video MER | ||
| 56 – 65 | Tele/Video MER | Tele MER, Subsequently targeted PPC. List of Tests – MER, Urine Routine, CBC with ESR, LFT, RFT, Lipid Profile, Hba1c, ECG | *MER, Urine Routine, CBC with ESR, LFT, RFT, Lipid Profile, Hba1c, ECG |
| 65-75 | *MER, Urine Routine, CBC with ESR, LFT, RFT, Lipid Profile, Hba1c, ECG |
| Above 75 | *MER, CBC ESR, HbA1c, Lipid Profile, Sr. Creatinine, SGOT, SGPT, Urine Routine, 2 D Echo, USG |
- *MER – Medical Examination Report,
- CBC – Complete Blood Count,
- ESR – Erythrocyte Sedimentation Rate ,
- LFT – Liver Function test,
- RFT – Renal Function Test,
- Hba1c – Hemoglobin A1C Test,
- ECG – Electro Cardiogram,
- PPC – Pre-Policy Check-up ,
- SGOT-Serum glutamic-oxaloacetic transaminase,
- SGPT- Serum glutamic pyruvic transaminase,
- USG- Ultrasound Sonography
– Port Proposals, Specially 56 – 65 age, targeted PPC will be advised after Tele / Video MER.
– In case of adverse medical declaration or portability, we may call for additional medical tests. We may conduct medical tests at diagnostic centre/ through home visit, based on medical disclosure wherever applicable.
– 100% of TeleMER cost would be borne by the Company, in case of proposal acceptance.
– *At least 50% of pre-policy medical checkup cost would be borne by Tata AIG in case where proposal is accepted.
– Financial underwriting may be done in case of higher sum insured options.
– The medical reports are valid for a period of 90 days from the date of Pre-Policy Checkup.
website www.tataaig.com.
Section 1 – Definitions
The terms defined below and at other junctures in the Policy Wording have the meanings ascribed to them wherever they appear in this Policy and where appropriate, references to the singular include references to the plural; references to the male includes other genders and references to any statutory enactment includes subsequent changes to the same.
i. Standard Definitions
1. Accident
An Accident means sudden, unforeseen and involuntary event caused by external, visible and violent means.
2. Any one Illness
Any one Illness means continuous period of Illness and includes relapse within 45 days from the date of last consultation with the Hospital/Nursing Home where treatment was taken.
3. AYUSH Day Care Centre
AYUSH Day Care Centre means and includes Community Health Centre (CHC), Primary Health Centre (PHC), Dispensary, Clinic, Polyclinic or any such health centre which is registered with the local authorities, wherever applicable and having facilities for carrying out treatment procedures and medical or surgical/para-surgical interventions or both under the supervision of registered AYUSH Medical Practitioner (s) on day care basis without in-patient services and must comply with all the following criterion:
i. Having qualified registered AYUSH Medical Practitioner(s) in charge;
ii. Having dedicated AYUSH therapy sections as required and/or has equipped operation theatre where Surgical Procedures are to be carried out;
iii. Maintaining daily records of the patients and making them accessible to the insurance company’s authorized representative.
4. AYUSH Hospital
An AYUSH Hospital is a healthcare facility wherein medical/surgical/para-surgical treatment procedures and interventions are carried out by AYUSH Medical Practitioner(s) comprising of any of the following:
a. Central or State Government AYUSH Hospital or
b. Teaching Hospital attached to AYUSH college recognized by the Central Government/ Central Council of Indian Medicine/ Central Council for Homeopathy, or
c. AYUSH Hospital, standalone or co-located with in-patient healthcare facility of any recognized system of medicine, registered with the local authorities, wherever applicable, and is under the supervision of a qualified registered AYUSH Medical Practitioner and must comply with all the following criterion:
i. Having atleast 5 in-patient beds;
ii. Having qualified AYUSH Medical Practitioner in charge round the clock;
iii. Having dedicated AYUSH therapy sections as required and/or has equipped operation theatre where Surgical Procedures are to be carried out;
iv. Maintaining daily records of the patients and making them accessible to the insurance company’s authorized representative.
5. AYUSH Treatment
AYUSH Treatment refers to the medical and / or Hospitalization treatments given under Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homeopathy systems.
6. Break in Policy
Break in Policy means the period of gap that occurs at the end of the existing Policy term/installment premium due date, when the premium due for Renewal on a given Policy or installment premium due is not paid on or before the premium Renewal date or Grace Period.
7. Cashless facility
Cashless facility means a facility extended by the Insurer to the insured where the payments, of the costs of treatment undergone by the insured in accordance with the Policy terms and conditions, are directly made to the Network Provider by the Insurer to the extent pre-authorization is approved.
8. Condition Precedent
Condition Precedent means a Policy terms or condition upon which the Insurer’s liability under the Policy is conditional upon.
9. Congenital Anomaly
Congenital Anomaly means a condition which is present since birth, and which is abnormal with reference to form, structure or position.
a. Internal Congenital Anomaly
Congenital Anomaly which is not in the visible and accessible parts of the body.
b. External Congenital Anomaly
Congenital Anomaly which is in the visible and accessible parts of the body.
10. Cumulative Bonus
Cumulative Bonus means any increase or addition in the Sum Insured granted by the Insurer without an associated increase in premium.
11. Day Care Centre
A Day Care Centre means any institution established for Day Care Treatment of Illness and/or injuries or a medical setup with a Hospital and which has been registered with the local authorities, wherever applicable, and is under supervision of a registered and qualified Medical Practitioner AND must comply with all minimum criterion as under –
i. has qualified nursing staff under its employment;
ii. has qualified Medical Practitioner/s in charge;
iii. has fully equipped operation theatre of its own where Surgical Procedures are carried out;
iv. maintains daily records of patients and will make these accessible to the insurance company’s authorized personnel.
12. Day Care Treatment
Day Care Treatment means medical treatment, and/or Surgical Procedure which is:
i. undertaken under General or Local Anesthesia in a Hospital/Day Care Centre in less than 24 hrs because of technological advancement, and
ii. which would have otherwise required Hospitalization of more than 24 hours. Treatment normally taken on an out-patient basis is not included in the scope of this definition.
13. Dental Treatment
Dental Treatment means a treatment related to teeth or structures supporting teeth including examinations, fillings (where appropriate), crowns, extractions and Surgery.
14. Domiciliary hospitalization
Domiciliary hospitalization means medical treatment for an Illness/disease/Injury which in the normal course would require care and treatment at a Hospital but is actually taken while confined at home under any of the following circumstances:
i. the condition of the patient is such that he/she is not in a condition to be removed to a Hospital, or
ii. the patient takes treatment at home on account of non-availability of room in a Hospital.
15. Emergency Care
Emergency Care means management for an Illness or Injury which results in symptoms which occur suddenly and unexpectedly, and requires immediate care by a Medical Practitioner to prevent death or serious long term impairment of the Insured Person’s health.
16. Grace Period
“Grace Period” means the specified period of time, immediately following the premium due date during which premium payment can be made to renew or continue a Policy in force without loss of continuity benefits pertaining to waiting periods and coverage of Pre-Existing Diseases.
For single premium payment policies, coverage is not available during the period for which no premium is received. However, If the premium is paid in instalments during the Policy Period, coverage will be available during the Grace Period, within the Policy Period.
The Grace Period for payment of the premium shall be: fifteen days where premium payment mode is monthly and thirty days in all other cases.
17. Hospital
A Hospital means any institution established for Inpatient Care and Day Care Treatment of Illness and/or injuries and which has been registered as a Hospital with the local authorities under Clinical Establishments (Registration and Regulation) Act 2010 or under enactments specified under the Schedule of Section 56(1) of the said act Or complies with all minimum criteria as under:
i. has qualified nursing staff under its employment round the clock;
ii. has at least 10 in-patient beds in towns having a population of less than 10,00,000 and at least 15 in-patient beds in all other places;
iii. has qualified Medical Practitioner(s) in charge round the clock;
iv. has a fully equipped operation theatre of its own where Surgical Procedures are carried out;
v. maintains daily records of patients and makes these accessible to the insurance company’s authorized personnel;
18. Hospitalization
Hospitalization means admission in a Hospital for a minimum period of 24 consecutive ‘Inpatient Care’ hours except for specified procedures/ treatments, where such admission could be for a period of less than 24 consecutive hours.
19. Illness
Illness means a sickness or a disease or pathological condition leading to the impairment of normal physiological function and requires medical treatment.
a. Acute condition
Acute condition is a disease, Illness or Injury that is likely to respond quickly to treatment which aims to return the person to his or her state of health immediately before suffering the disease/ Illness/ Injury which leads to full recovery
b. Chronic condition
A chronic condition is defined as a disease, Illness, or Injury that has one or more of the following characteristics:
i. it needs ongoing or long-term monitoring through consultations, examinations, check-ups, and /or tests
ii. it needs ongoing or long-term control or relief of symptoms
iii. it requires rehabilitation for the patient or for the patient to be specially trained to cope with it
iv. it continues indefinitely
v. it recurs or is likely to recur
20. Injury
Injury means accidental physical bodily harm excluding Illness or disease solely and directly caused by external, violent, visible and evident means which is verified and certified by a Medical Practitioner.
21. Inpatient Care
Inpatient Care means treatment for which the Insured Person has to stay in a Hospital for more than 24 hours for a covered event.
22. Intensive Care Unit:
Intensive Care Unit means an identified section, ward or wing of a Hospital which is under the constant supervision of a dedicated Medical Practitioner(s), and which is specially equipped for the continuous monitoring and treatment of patients who are in a critical condition, or require life support facilities and where the level of care and supervision is considerably more sophisticated and intensive than in the ordinary and other wards.
23. ICU Charges:
ICU (Intensive Care Unit) Charges means the amount charged by a Hospital towards ICU expenses which shall include the expenses for ICU bed, general medical support services provided to any ICU patient including monitoring devices, critical care nursing and intensivist charges.
General Note: An intensivist is a board-certified physician who provides special care for critically ill patients.
24. Maternity Expenses:
Maternity Expenses means;
a. medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean sections incurred during Hospitalization);
b. expenses towards lawful medical termination of pregnancy during the Policy Period.
25. Medical Advice
Medical Advice means any consultation or advice from a Medical Practitioner including the issuance of any prescription or follow-up prescription.
26. Medical Expenses:
Medical Expenses means those expenses that an Insured Person has necessarily and actually incurred for medical treatment on account of Illness or Accident on the advice of a Medical Practitioner, as long as these are no more than would have been payable if the Insured Person had not been insured and no more than other Hospitals or doctors in the same locality would have charged for the same medical treatment.
27. Medical Practitioner
Medical Practitioner means a person who holds a valid registration from the Medical Council of any State or Medical Council of India or Council for Indian Medicine or for Homeopathy set up by the Government of India or a State Government and is thereby entitled to practice medicine within its jurisdiction; and is acting within its scope and jurisdiction of license.
28. Medically Necessary Treatment
Medically Necessary Treatment means any treatment, tests, medication, or stay in Hospital or part of a stay in Hospital which:
i. is required for the medical management of the Illness or Injury suffered by the insured;
ii. must not exceed the level of care necessary to provide safe, adequate and appropriate medical care in scope, duration, or intensity;
iii. must have been prescribed by a Medical Practitioner;
iv. must conform to the professional standards widely accepted in international medical practice or by the medical community in India.
29. Migration
“Migration” means a facility provided to policyholders (including all members under family cover and group policies), to transfer the credits gained for Pre-Existing Diseases and specific waiting periods from one health insurance Policy to another with the same Insurer.
30. Network Provider
Network Provider means Hospitals or health care providers enlisted by an Insurer, TPA or jointly by an Insurer and TPA to provide medical services to an insured by a Cashless facility.
The updated list of Network Provider is available on Our website (www.tataaig.com).
31. New Born Baby
New Born Baby means baby born during the Policy Period and is aged upto 90 days.
32. Non-Network Provider
Non-Network means any Hospital, Day Care Centre or other provider that is not part of the network.
33. Notification of Claim
Notification of Claim means the process of intimating a claim to the Insurer or TPA through any of the recognized modes of communication.
34. OPD treatment
OPD treatment means the one in which the Insured visits a clinic / Hospital or associated facility like a consultation room for diagnosis and treatment based on the advice of a Medical Practitioner. The Insured is not admitted as a day care or in-patient.
35. Pre-Existing Disease
“Pre-Existing Disease (PED)” means any condition, ailment, Injury or disease:
a. that is/are diagnosed by a physician not more than 36 months prior to the date of commencement of the Policy issued by the Insurer; or
b. for which Medical Advice or treatment was recommended by, or received from, a physician, not more than 36 months prior to the date of commencement of the Policy.
36. Pre-hospitalization Medical Expenses
Pre-hospitalization Medical Expenses means Medical Expenses incurred during predefined number of days preceding the Hospitalization of the Insured Person, provided that:
i. Such Medical Expenses are incurred for the same condition for which the Insured Person’s Hospitalization was required, and
ii. The In-patient Hospitalization claim for such Hospitalization is admissible by the Insurance Company.
37. Portability
“Portability” means a facility provided to the health insurance policyholders (including all members under family cover), to transfer the credits gained for, Pre-Existing Diseases and specific waiting periods from one Insurer to another Insurer.
38. Post-hospitalization Medical Expenses
Post-hospitalization Medical Expenses means Medical Expenses incurred during predefined number of days immediately after the Insured Person is discharged from the Hospital provided that:
i. Such Medical Expenses are for the same condition for which the Insured Person’s Hospitalization was required, and
ii. The inpatient Hospitalization claim for such Hospitalization is admissible by the insurance company.
39. Qualified Nurse
Qualified Nurse means a person who holds a valid registration from the Nursing Council of India or the Nursing Council of any state in India.
40. Reasonable and Customary charges
Reasonable and Customary charges means the charges for services or supplies, which are the standard charges for the specific provider and consistent with the prevailing charges in the geographical area for identical or similar services, taking into account the nature of the Illness / Injury involved.
General Note: to avoid unnecessary stress better go to network hospitals)
41. Renewal
Renewal means the terms on which the contract of insurance can be renewed on mutual consent with a provision of Grace Period for treating the Renewal continuous for the purpose of gaining credit for Pre-Existing Diseases, time-bound exclusions and for all waiting periods.
42. Room Rent
Room Rent means the amount charged by a Hospital towards Room and Boarding expenses and shall include the Associated Medical Expenses.
43. Surgery or Surgical Procedure
Surgery or Surgical Procedure means manual and / or operative procedure (s) required for treatment of an Illness or Injury, correction of deformities and defects, diagnosis and cure of diseases, relief from suffering and prolongation of life, performed in a Hospital or Day Care Centre by a Medical Practitioner.
44. Unproven/Experimental treatment
Unproven/Experimental treatment means the treatment including drug experimental therapy which is not based on established medical practice in India, is treatment experimental or unproven.
ii. Specific Definitions (Definitions other than as mentioned under Section 1 (i) above)
1. Age
Means the completed Age of the Insured Person on his / her last birthday as on date of commencement of the Policy and as per the English calendar.
2. Aggregate Deductible
Aggregate Deductible is a cost sharing requirement under this Policy which provides that We will not be liable for a specified amount in aggregate for all claims during the per Policy Year. A deductible does not reduce the Sum Insured.
3. Associated Medical Expenses (AME)
AME shall include nursing charges, operation theatre charges, fees of Medical Practitioner/surgeon/ anesthetist/ specialist (excluding cost of pharmacy and consumables, cost of implants and medical devices, cost of diagnostics) conducted within the same Hospital where the Insured Person has been admitted. It shall not be applicable for Hospitalization in ICU. Associated Medical Expenses shall be applicable for covered expenses, incurred in Hospitals which follow differential billing based on the room category.
4. Multi-Sharing Accommodation
Multi-Sharing Accommodation means a Hospital room with three or more patient beds. This definition does not apply to ICU or ICCU.
5. Modern Treatment Methods and Advancement in Technologies
The following Procedures shall be considered for Modern Treatment Methods and Advancement in Technologies: (12)
A. Uterine Artery Embolization and HIFU
B. Balloon Sinuplasty
C. Deep Brain stimulation
D. Oral chemotherapy
E. Immunotherapy-Monoclonal Antibody to be given as injection
F. Intra vitreal injections
G. Robotic surgeries
H. Stereotactic radiosurgeries
I. Bronchical Thermoplasty
J. Vaporisation of the prostrate (Green laser treatment or holmium laser treatment)
K. IONM – (Intra Operative Neuro Monitoring)
L. Stem cell therapy: Hematopoietic stem cells for bone marrow transplant for haematological conditions to be covered.
6. Policy
Policy means the contract of insurance including but not limited to Policy Schedule, Endorsements,
Policy Wordings (inbuilt covers & optional covers, if opted), Riders, Annexures etc., as applicable.
7. Policy Period
Policy Period means the time during which this Policy is in effect. Such period commences from Commencement Date and ends on the Expiry Date and specifically appears in the Policy Schedule.
8. Policy Schedule
Policy Schedule means the Policy Schedule attached to and forming part of Policy.
9. Policy Year
Policy Year means a period of twelve consecutive months beginning from the date of commencement of the Policy Period and ending on the last day of such twelve-month period.
For the purpose of subsequent years, Policy Year shall mean a period of twelve months commencing from the end of the previous Policy Year and lapsing on the last day of such twelve-month period, or the Policy Expiry date whichever is earlier.
10. Single Private Room
Single Private Room means an air-conditioned room in a Hospital where a single patient is accommodated and which has an attached toilet (lavatory and bath). Such room type shall be the most basic and the most economical of all accommodations available as a single occupancy room in that Hospital.
This does not include a deluxe room or a suite or a VIP room. Any room that offers services or incurs charges greater than those of the Single Private Room shall be classified as a room category higher than the Single Private Room.
11. Sum Insured
“Sum Insured” refers to the amount specified in the Policy Schedule at the inception of a Policy Year, excluding any Bonus. Sum Insured represents Our maximum, total and cumulative liability under the Policy, for all the Insured Person(s) covered in aggregate, for the respective Policy Year.
• Upon the successful admission of a claim, the Sum Insured for the remaining Policy Year shall be accordingly reduced by the amount of the claim settled (inclusive of ‘taxes’) or admitted.
• In cases where the Policy Period is 2/3 years, the specified Sum Insured in the Policy Schedule signifies the limit for the initial Policy Year. This limit shall expire at the conclusion of the first year, and fresh limit up to the opted Sum Insured will become available for the subsequent second/third year, unless specified otherwise
12. Twin Sharing Accommodation
Twin Sharing Accommodation means a Hospital room with two patient beds. This definition does not apply to ICU or ICCU. Such room type shall be the most basic and the most economical of all accommodations available as twin sharing room in that Hospital.
13. We, Us, Our, Insurer
means The TATA AIG General Insurance Company Limited that has provided Insurance Cover under this Policy.
14. You, Your, Insured Person
means the person whose name specifically appears in the Policy Schedule as an Insured Person/ Policyholder.
15. Zone(s)
For the purpose of premium computation, the country is divided into following three Zones and premium payable under this Policy will be computed based on the Zone as applicable for the ‘Address’ of the proposer/ Insured Person:
• Zone A: Mumbai (including Mumbai Metropolitan Region), Delhi (including National Capital Region, Faridabad, Ghaziabad), Ahmedabad, Surat, Baroda and Hisar
• Zone B: Hyderabad (including Secunderabad), Sangareddy, Bengaluru, Kolkata (including Kolkata Metropolitan Area, Howrah, Hoogly), Indore, Gwalior, Chennai, Chandigarh (including, Mohali, Punchkula, Zirakpur), Pune (including Pimpri Chinchwad), Rajkot, Gandhinagar, Patan, Mahesana, Sabarkantha, Banaskantha, Junagadh, Navsari, Kheda, Arvalli, Mahisagar, and Surendranagar
• Zone C: Rest of India
Here ‘Address’ implies the place where the person ordinarily resides. In case proposed prospect(s) reside at multiple addresses, then address of the person residing in the highest Zone will be considered.
Please note that the above-mentioned categorization of zones is subject to change at Our sole discretion. Any such change made which shall impact an existing policyholder, shall be intimated under 3 months’ notice and shall be applicable from the immediate next Renewal.
Section 2 – Benefits
If during the Policy Period one or more Insured Person(s) is required to be hospitalized for treatment (including Modern Treatment Methods and Advancement in Technologies) of an Illness or Injury at a Hospital / Day Care Centre, following Medical Advice of a duly qualified Medical Practitioner, the Company shall indemnify Medically Necessary expenses towards the coverage mentioned in the Policy Schedule for the amount of such Reasonable and Customary charges or compensate to the extent agreed, upto the limits mentioned, subject to terms and conditions of the Policy . Provided further that, any amount payable under the Policy shall be subject to the terms of coverage (including Aggregate Deductible, if opted), exclusions, conditions and definition contained herein. Maximum liability of the Company under all such Claims during each Policy Year shall be the Sum Insured opted and Cumulative Bonus (if accrued), as specified in the Policy Schedule (except in case of a claim under Infinite Advantage (if opted) or Early Access (if opted)).
In case of family floater Policy, the Sum Insured, Cumulative Bonus & Aggregate Deductible, if applicable, shall be available for all Insured Persons on an aggregate basis, on a per Policy Year basis.
B1. In-Patient Treatment
We will cover Medical Expenses for Medically Necessary Treatment in a Hospital due to disease/Illness/Injury (covered event), for period more than 24 hrs., that requires an Insured Person’s admission in a Hospital for an Inpatient Care, during the Policy Period.
Medical Expenses directly related to the Hospitalization would be payable.
The Company shall indemnify Medical Expenses as listed below:
i. Room Rent, Boarding, Nursing Expenses as provided by the Hospital / Nursing Home, up to the room category specified in the Policy Schedule.
ii. Intensive Care Unit (ICU) / Intensive Cardiac Care Unit (ICCU) expenses
iii. Surgeon, Anesthetist, Medical Practitioner, Consultants, Specialist Fees
iv. Anesthesia, Qualified Nurse charges, blood, oxygen, operation theatre charges, surgical appliances, medicines, drugs, costs towards diagnostics, diagnostic imaging modalities and such similar other expenses.
If the Insured Person is admitted in a room whose category is higher than the one that is specified in the Policy Schedule, then the Insured Person shall bear a rateable proportion of the Room Rent and the total Associated Medical Expenses, including surcharge or taxes thereon in the proportion of the ‘difference between the Room Rent actually incurred & the Room Rent of the entitled room category’ to ‘the Room Rent actually incurred’.
• Proportionate deductions are not applicable for ICU Charges.
• Such proportionate deductions, if any, will not be applied in respect of the Hospitals which do not follow differential billing or for those Associated Medical Expenses in respect of which differential billing is not adopted based on the room category.
Benefit Specific Sub-limit: Room Category –Upto Single private room. For category applicable to you, please refer your Policy Schedule.
Limit for In-Patient Treatment- Upto Sum Insured
B2. Pre-Hospitalization expenses
We will cover expenses for pre-hospitalization consultations, investigations and medicines incurred upto 90 days prior to the date of admission to the Hospital. Any pre-hospitalization expenses incurred prior to Policy Period shall not be covered.
The benefit is payable if We have admitted a claim under B1, B4, or B6.
Limit for Pre-Hospitalization expenses- Upto 90 days, Upto Sum Insured
B3. Post-Hospitalization expenses
We will cover expenses for post-hospitalization consultations, investigations and medicines incurred upto 90 days after discharge from the Hospital.
The benefit is payable if We have admitted a claim under B1, B4, or B6.
Limit for Post-Hospitalization expenses- Upto 90 days, Upto Sum Insured
B4. Day Care Procedures
We will cover expenses for Day Care Treatment, due to disease/Illness/Injury (covered event), taken in a Hospital or a Day Care Centre, during the Policy Period.
Limit for Day Care Procedures- Upto Sum Insured
B5. Organ Donor
We will cover the Medical Expenses, incurred by or in respect of the organ donor, for an organ transplant Surgery, solely towards the harvesting of the organ donated subject to the following conditions:
i. The organ donation conforms to the Transplantation of Human Organs (Amendment) Bill, 2011 and the organ is for the use of the Insured Person;
ii. The Insured Person is the recipient of the organ so donated by the organ donor and the claim of such Surgery is accepted by Us under B1 of this Policy;
iii. The organ transplant is medically necessary for the Insured Person as certified by a Medical Practitioner
iv. Claim under this section shall be assessed as per the claim of the recipient Insured Person
What is not covered (Addl. Information compared to premier)
i. Pre-hospitalization Medical Expenses or Post hospitalization Medical Expenses of the organ donor
ii. Screening Expenses of the organ donor
iii. Any other medical expense as a result of harvesting from the organ donor
iv. Costs directly or indirectly associated with the acquisition of the donor’s organ.
v. Transplant of any organ/tissue where the transplant is experimental or investigational
vi. Expenses related to organ transportation or preservation
vii. Any other medical treatment or complication in respect of the donor, consequent to harvesting.
Limit for Organ Donor- Upto Sum Insured
B6. Domiciliary Treatment
We will cover expenses related to Domiciliary hospitalization of the Insured Person if the treatment exceeds beyond three consecutive days and is availed during the Policy Period. The treatment must be for management of an Illness and not for enteral feedings or end of life care.
At the time of claiming under this benefit, We shall require certification from the treating doctor fulfilling the conditions as mentioned under the general definitions (Section 1) of this Policy.
Limit for Domiciliary Treatment- Upto Sum Insured
B7. AYUSH Benefit
We will cover Medical Expenses incurred for treatment as In-Patient or Day Care in an AYUSH Hospital/ AYUSH Day Care Centre, for a room category, as specified in the Policy Schedule and applicability of Associated Medical Expenses.
This benefit shall also cover Pre-hospitalization Medical Expenses for a period of upto 90 days before the date of admission to the AYUSH Hospital/ AYUSH Day Care Centre and Post-hospitalization Medical Expenses for a period upto 90 days, subject to AYUSH In-Patient Hospitalization or AYUSH Day Care Treatment claim being admissible under this benefit.
Claims under this section shall be assessed as per the applicable insurance guidelines related to AYUSH and benchmark rates as available on Ministry of AYUSH website (https://ayushnext.ayush.gov.in/site/insurance-guidelines-related-to-ayush).
For reference, please refer the document “Annexure B for AYUSH Benefit” available on Our website (www.tataaig.com)
Limit for AYUSH Benefit- Upto Sum Insured
B8. Ambulance Cover (Road)
We will cover expenses incurred for the transportation of the Insured Person in a registered road ambulance, within a radius of 50 kilometers, (Addl. Information compared to premier) for the following:
i. In case of an emergency, from site of incident to the nearest Hospital for admission
ii. If medically necessary and prescribed by the treating practitioner, from Insured Person’s residence to Hospital
iii. From one Hospital to another Hospital for better medical facilities and treatment or from one Hospital to diagnostic center for advanced diagnostic treatment, where such facility is not available at the existing Hospital.
iv. If medically necessary and prescribed by the treating practitioner, from Hospital to Insured Person’s residence
For this claim to be paid, the claim must be admissible under B1 or B4 of this Policy.
Limit for Ambulance Cover- Upto Sum Insured
B9. Restore Infinity Plus (- for both Related + Unrelated)
We will provide reinstatement of the base Sum Insured, if the Sum Insured and Cumulative Bonus (if accrued) is insufficient to pay an admissible Hospitalization claim in the Policy. The reinstatement will be available for unlimited number of times during a Policy Year, subject to below conditions:
i. This benefit shall not be available for the first admissible Hospitalization/ Domiciliary Treatment claim in each Policy Year. The Sum Insured will be restored for the subsequent claim in the Policy Year.
ii. In case of Family Floater Policy, reinstatement of Sum Insured will be available for all Insured Persons in the Policy on floater basis.
iii. The unutilized restored Sum Insured cannot be carried forward to the next Policy Year.
iv. This benefit shall also be applicable annually for policies with tenure of more than 1 year.
v. Any restored Sum Insured can only be utilized for an admissible claim under following indemnity covers of the Policy, as applicable:
a. In-Patient Treatment,
b. Pre/Post Hospitalization expenses,
c. Day Care Procedures,
d. Organ donor,
e. Domiciliary Treatment,
f. AYUSH Benefit,
g. Ambulance Cover,
h. Consumable benefit (If opted)
vi. Any restored Sum Insured under this benefit cannot be utilized for an admissible claim under:
a. Any cover other than the ones mentioned in the above section or
b. Any cover which has Sum Insured over and above the base Sum Insured.
vii. Our maximum liability in aggregate of all claims arising out of a single Hospitalization shall not exceed the Sum Insured of the base Policy.
Note: No 45 Days waiting period or Restriction on Dialysis or Cancer Treatment.
B10. Daily Cash for choosing Twin Sharing Accommodation
We will pay a fixed amount per day as mentioned in the Policy Schedule, if the Insured Person is Hospitalized in a Twin Sharing Accommodation (2 Patients), for each continuous and completed period of 24 hours.
Payout under this benefit is only available if the room category eligibility applicable under this Policy is ‘Single Private Room’ or room category higher than the Single Private Room.
This benefit has a separate limit (over and above base Sum Insured) and does not affect No Claim Bonus.
Optional Sub-limit: Twin Sharing accommodation — Room Category Select
Limit for Daily Cash for choosing Twin Sharing Accommodation- Rs.1200 per day (over and above base sum insured)
B11. Daily Cash for choosing Multi-Sharing Accommodation
We will pay a fixed amount per day as mentioned in the Policy Schedule, if the Insured Person is Hospitalized in a Multi-Sharing Accommodation (More Than 2 Patients) , for each continuous and completed period of 24 hours.
Payout under this benefit is only available if the room category eligibility applicable under this Policy is ‘Single Private Room’ or room category higher than the Single Private Room.
This benefit has a separate limit (over and above base Sum Insured) and does not affect No Claim Bonus.
Limit for Daily Cash for choosing Multi-Sharing Accommodation- Rs.1500 per day (over and above base sum insured)
Note: Sharing Room Discount is not suggested to Opt, as during Hospitalization, mostly you will go to Single Room only then you have to pay CO-Pay.
B12. No Claim Bonus
Note: if you opt for Super Charge Bonus then this benefit wont be applicable.
Under this section, the below mentioned ‘No claim Bonus’ options will be available and applicable as opted by You.
Cumulative bonus or Discount in Renewal Premium will be available for every claim free policy year.
Either of the two options is to be selected:
1) Cumulative Bonus
i. 50% Cumulative Bonus will be applied on the Sum Insured of the expiring Policy, on each Renewal after every claim free Policy Year, provided that the Policy is renewed with Us and without a break. The maximum Cumulative Bonus shall not exceed 100% of the Sum Insured in any Policy Year.
ii. If a Cumulative Bonus has been applied and a claim is made, then in the subsequent Policy Year We will automatically decrease the Cumulative Bonus by 50% of the Sum Insured in that following Policy Year. There will be no impact on the base Sum Insured, only the accrued Cumulative Bonus will be decreased.
iii. In policies with a tenure of more than one year, the above guidelines of Cumulative Bonus shall be applicable post completion of each Policy Year.
iv. In relation to a Family Floater, the Cumulative Bonus so applied will only be available in respect of those Insured Person(s) who were Insured Person(s) in the claim free Policy Year and continue to be Insured Person(s) in the subsequent Policy Year.
v. For the purpose of computation of Cumulative Bonus, the percentage (%) of Cumulative Bonus will be applied on the base Sum Insured of the expiring Policy only. The Restore Infinity Plus amount will not be taken into consideration for such computation.
vi. Reduction of Sum Insured: In case the Sum Insured under the Policy is reduced at the time of Renewal then the accrued Cumulative Bonus under this benefit shall be reduced in proportion to the reduced Sum Insured.
vii. Cumulative Bonus will lapse if the Policy is not renewed before Policy expiry (including the Grace Period).
2) Discount in Renewal Premium (No Claim Bonus): (Not Suggested)
If you choose Discount in Renewal Premium, We will allow 1% discount on renewal premium for every claim free Policy Year, provided that the Policy is renewed with Us without break.
Tax Benefit:
The premium amount paid under this policy qualifies for deduction under Section 80D of the Income Tax Act.
Optional Covers
The Optional Cover(s) can only be opted along with the base covers under the Policy and cannot be opted in isolation or as a separate product. The Optional cover(s) are provided on payment of additional premium or discounts and subject to the terms and conditions and exclusions as stated in the Policy Terms and Conditions and Exclusions. These Optional Cover(s), if selected, should be opted for all eligible Insured Persons to be covered under the Policy unless stated otherwise and shall be available only if the same are specifically mentioned in the Policy Schedule.
The insurance provided under these Optional cover(s) are only with respect to such and so many of the coverages as are indicated in the Policy Schedule.
C1. Consumables Benefit (Must & Should Opt)
In consideration of additional premium paid and notwithstanding the exclusion mentioned under Section 3.ii (Specific Exclusions).A.(xii), if this optional cover has been opted, We will cover expenses incurred for specified consumables, subject to balance Sum Insured, which are mentioned in Annexure I – List I of optional items (Consumables Benefit) available on Our website (www.tataaig.com) which are consumed during the period of Hospitalization directly related to the Insured Person’s medical or surgical treatment of Illness/disease/Injury.
Conditions applicable for claim to be admissible under this cover:
o Item is a medical consumable and is medically necessary;
o prescribed by the treating Medical Practitioner and
o the Hospitalization claim is admissible under B1 or B4 of this Policy.
The assessment of payout under this Optional Cover shall follow the assessment of claim done under B1 and B4 except for application of Associated Medical Expenses.
Limit for Consumables Benefit- Upto Sum Insured
C2. Maternity Care (for All 3)
In consideration of additional premium paid and if this optional cover has been opted, We will cover Maternity Expenses, delivery complication of a New Born Baby and First Year Vaccinations of the New Born Baby up to the limits specified in the Policy Schedule.
This benefit has a separate limit (over and above base Sum Insured) and does not affect No Claim Bonus.
The cover is available for the selected Insured Person(s) and is subject to a waiting period of 2 years of continuous coverage of the Insured Person(s) under this cover with Us.
i. Maternity Expenses:
Notwithstanding the exclusion mentioned under Section 3.i (Standard Exclusions).B.(xii) Maternity (Code – Excl 18), We will cover Maternity Expenses related to childbirth and lawful medical termination of pregnancy during the Policy Period.
We will not cover ectopic pregnancy under this benefit; however, it shall be covered under section B1.
The following shall be excluded from the scope of this coverage:
• Expenses incurred for pre/post natal care
• Pre/Post Hospitalization Expenses (Section B2 and B3 of this Policy)
Also, no coverage is available for voluntary termination of pregnancy during the Policy Period under this Policy.
ii. Delivery Complications of New Born Baby:
For complications related to delivery, We will cover Medically Necessary Treatment of the New Born Baby incurred during the Hospitalization, if claim related to childbirth is admissible under the ‘Maternity Expenses’ cover (C2. i) of this Policy.
iii. First year Vaccinations:
We will cover vaccination expenses for the child up to their first birthday, if claim related to childbirth is admissible under the ‘Maternity Expenses’ cover (C2. i) of this Policy and subject to continuity of the Policy with Us.
The limit available under this benefit is a lifetime limit for each child.
Limit for Maternity Care (all 3 ) – 10% of Sum Insured, maximum up to Rs.1,00,000 per policy year (over and above base sum insured)
C3. Reduction of Maternity Care Waiting Period
In consideration of additional premium paid, the waiting period specified under Section C2 of this Policy shall be reduced to 1 year of continuous coverage.
C4. Infinite Advantage
no limit on the Sum Insured for one claim
In consideration of additional premium paid, We will cover the Medical Expenses incurred for an admissible claim under In-Patient Treatment/Daycare Procedures for any one claim during the lifetime of the Policy, without any limits on the available annual Sum Insured, subject to the following conditions:
i. The cover can be selected only at the inception of the Policy. Once opted, the cover has to be opted continuously under the Policy, until a claim is made under this cover.
ii. All the conditions applicable for the admissibility of In-Patient Treatment/Daycare Procedures cover shall be applicable to this cover
iii. This cover is applicable only for one claim in the lifetime of the Policy.
iv. Once a claim has been made under this Cover, the cover will cease to exist and cannot be opted again upon subsequent Renewals.
v. The available amount shall be utilized as per following sequence in event of a claim under this Optional Cover:
a. Base Sum Insured/ Early Access (if opted)
b. Cumulative Bonus
c. Infinite Advantage (only when the total amount available for claim is exhausted)
vi. After utilization of all the above-mentioned benefits, the total available amount shall be reduced to zero for that Policy Year/tenure (If Early Access has been opted) following the payment of claim under Infinite Advantage.
vii. Room category applicable under this cover shall be as per the room category opted and mentioned in the Policy Schedule
viii. ‘Aggregate Deductible’ or any other cost sharing covers, if opted, shall be applicable under this cover.
C5. Early Access
In consideration of additional premium paid, for single premium multi-year policies, the Sum Insured of the Policy Period shall be available anytime during the Policy Period, for utilization towards an admissible claim under Section B1, B2, B3, B4, B5, B6, B7 or B8.
With Early Access: Your annual Base Sum Insured is combined for the entire tenure opted by You. This combined Base Sum Insured will be available for the entire Policy tenure which means that unutilized Sum Insured, if any, shall be carried forward to the next Policy Year of the same Policy Period.
Illustration
Base Sum Insured (per Policy Year): Rs. 20 Lakhs
Policy Tenure: 3 Years
| Year | Without Early Access | With Early Access |
| Sum Insured (Rs.) | ||
| Year 1 | 20 Lakhs | 60 Lakhs |
| Year 2 | 20 Lakhs | |
| Year 3 | 20 Lakhs | |
| Year 4 | 20 Lakhs | 60 Lakhs |
| Year 5 | 20 Lakhs | |
| Year 6 | 20 Lakhs | |
Explanation:
Without Early Access: If You purchase a Policy of tenure of more than 1 year, Your Policy Sum Insured operates on annual basis. Which means if You have a Policy of Base Sum Insured Rs. 20 Lakhs, You can use Rs. 20 Lakhs in each Policy Year towards admissible claims.
C6. Room Category Select (For HNI)
Any Room (For HNI) Addl premium has to pay or TWIN Sharing Accommodations – Get Discount (not Recommended)
If this optional cover is availed, the room category entitlement in the Policy shall be replaced to the room category as specified in the Policy Schedule.
However, if the Insured Person is admitted in a room whose category is higher than the one that is specified in the Policy Schedule, then the Insured Person shall bear a rateable proportion of the Room.
Rent and the total Associated Medical Expenses, including surcharge or taxes thereon in the proportion of the ‘difference between the Room Rent actually incurred & the Room Rent of the entitled room category’ to ‘the Room Rent actually incurred’.
• Proportionate deductions are not applicable for ICU Charges.
• Such proportionate deductions, if any, will not be applied in respect of the Hospitals which do not follow differential billing or for those Associated Medical Expenses in respect of which differential billing is not adopted based on the room category.
C7. Aggregate Deductible (if you don’t want to claim small amounts)
10K / 25K / 50K / 100K
In consideration of premium discount availed by You, Our liability under this Policy shall be subject to Aggregate Deductible as specified in the Policy Schedule, subject to the following conditions:
i. Aggregate Deductible, shall be applicable on aggregate of final assessed amount of all admissible claims in a Policy Year and Our liability shall be restricted to the balance amount, subject to availability of Sum Insured
ii. In case of multi-year base Policy (i.e. tenure more than 1 year), such Aggregate Deductible would be applicable per Policy Year.
iii. Aggregate Deductible shall be applicable for all indemnity claims under following covers of this Policy, as applicable:
a. In-Patient Treatment,
b. Pre/Post Hospitalization expenses,
c. Day Care Procedures,
d. Organ donor,
e. Domiciliary Treatment,
f. AYUSH Benefit,
g. Ambulance Cover
h. Consumable benefit (if opted)
i. Infinite Advantage (if opted)
j. Early Access (if opted)
C8. Introduction of Valued Provider Network (not Suggested)
Any treatment availed outside Our network of “Valued Provider-Pan India” shall attract a Co-Payment of 30% for each such claim, resulting from admission of the Insured Person in a Hospital/ Day Care Centre/ AYUSH Hospital
Discounts on premium:
| A | Long term discount | 7.5% for a policy term of 3 years 5% for a policy term of 2 years This discount is available only with ‘Single’ Premium Payment mode. | ||||
| B | Family floater discount | 1 member | No Discount | |||
| 2 members | 22% | |||||
| 3 members | Atleast 1 child | 28% | ||||
| No child | 22% | |||||
| 3+ members | Atleast 2 children | 32% | ||||
| Atleast 1 child | 28% | |||||
| No child | 22% | |||||
| C | Multi- Individual Discount | 5% (When more than one member are covered in a policy on individual basis) | ||||
| D | Professional Discount | 7.5% (This discount is applicable for salaried employee of public or a private company) | ||||
| E | Young Family Discount | 10% 1. This discount is applicable only if all the Insured Persons covered are of age of 40 years or below at the time of first inception of the policy. 2. This discount will be effective from the first year of the policy and will continue for the lifetime of the policy, irrespective of claims. 3. This discount will be discontinued if, at any point during the policy year, a new member is added whose entry age in policy is 40 years or above. | ||||
| F | Discount in lieu of commission | Upto 15% |
| G | Favorable Experience Discount | 20% at the inception of the policy. At Renewal, the Favorable Experience Discount may vary based on established criteria. |
Favorable Experience Discount:
At Renewal, the Favorable Experience Discount will depend on below criteria:
| Claim Years in last 3 Policy Years | Discount |
| 3 Years | 0% |
| 2 Years | 5% |
| 1 Year | 10% |
| No Claim | 20% |
Note:
Where ‘Claim Year’ is a Policy year in which one or more claim(s) have been paid. For the purpose of Favorable Experience Discount, a Policy year with claim only under ‘Daily Cash for choosing Twin Sharing Accommodation’, ‘Daily Cash for choosing Multi-Sharing Accommodation’ and ‘Maternity Care’ benefit will not be considered a ‘Claim Year’.
Note: The above mentioned discounts are multiplicative and applied on the base premium. Discounts other than Long term discount, Family floater discount, Multi-Individual Discount, Favorable Experience Discount and Discount in Renewal Premium (No Claim Bonus) are subject to a maximum cap of 25%.
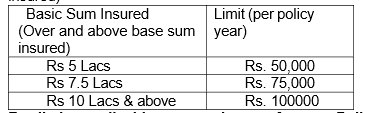
C 9.Supercharge Bonus Rider
We will provide Supercharge Bonus in the form of specified percentage of the base Sum Insured of the expiring Policy, post completion of each Policy Year, irrespective of claims in preceding Policy Years. The total accrued Supercharge Bonus shall not exceed specified percentage of the base Sum Insured in any Policy Year.
Get bonus of 100% of Sum Insured every year, irrespective of claims; Max up to specified percentage of base sum insured.
Inbuilt for Sum insured of Rs.5 Lakhs to Rs. 7.5Lakhs, 100% per policy year, Max up to 300%.
Optional: for Sum Insured of Rs.10Lakhs & above , 100% per policy year, Max up to 300%.
Note: Supercharge Bonus Rider will override the “No claim Bonus” benefit under the product. i.e if you opt this Riders then NCB won’t applicable.
Home Care Treatment Rider
We’ll cover the cost of expenses up to sum insured, incurred for treatment taken at home. The pandemic care will be covered upto 25% of the sum insured.
Accidental Death Benefit Rider
If an Insured Person suffers an accident during the policy period and this is the sole and direct cause of his death within 365 days from the date of accident, then we will pay 100% of the Sum Insured or Rs. 50,00,000, whichever is lower
Advanced Cover Rider (Not Available)
Cut the waiting period for specific pre-existing diseases to just 30 days for faster access to treatment.
Preventive Annual Health Checkup Rider (Not Available)
Get cashless annual health check-ups at home or with our providers, keeping health in check every year, ensuring proactive health management.
OPD Care (Not Available)
Get coverage for OPD Consultation, Dental, Vision and teleconsultations for seamless Outpatient Care.
EmpowerHer (Not Available)
Comprehensive coverage for women’s health, from gynaecologist visits and PCOD treatment to cancer screenings and vaccinations.
Mental Wellbeing (Not Available)
Holistic mental health care with mental health screenings, psychological therapy, stress management, diet consultations, and addiction cessation programs.
Cancer Care:
Suggested only if Family Tree has effected with Cancer.
Section 3 – Exclusions
We will neither be liable nor make any payment for any claim in respect of any Insured Person which is caused by, arising from or in any way attributable to any of the following exclusions. All the waiting periods shall be applicable individually for each Insured Person.
i. Standard Exclusions
A. Exclusions with waiting periods
i. Pre-Existing Diseases Waiting Period (Code- Excl 01):
a. Expenses related to the treatment of a Pre-Existing Disease (PED) and its direct complications shall be excluded until the expiry of 36 months of continuous coverage after the date of inception of the first Policy with Us.
b. In case of enhancement of Sum Insured the exclusion shall apply afresh to the extent of Sum Insured increase.
c. If the Insured Person is continuously covered without any break as defined under the Portability norms of the extant IRDAI (Health Insurance) Regulations, then waiting period for the same would be reduced to the extent of prior coverage.
d. Coverage under the Policy after the expiry of 36 months for any Pre-Existing Disease is subject to the same being declared at the time of application and accepted by Us.
ii. (40 + 1) Specified Disease/Procedure Waiting Period (Code- Excl 02):
(Not applicable for claims arising due to an accident)
a. Expenses related to the treatment of the listed conditions, surgeries/treatments shall be excluded until the expiry of 24 months of continuous coverage after the date of inception of the first Policy with Us. This exclusion shall not be applicable for claims arising due to an Accident.
b. In case of enhancement of Sum Insured, the exclusion shall apply afresh to the extent of Sum Insured increase.
c. If any of the specified disease/procedure falls under the waiting period specified for Pre- Existing Diseases, then the longer of the two waiting periods shall apply.
d. The waiting period for listed conditions shall apply even if contracted after the Policy or declared and accepted without a specific exclusion.
e. If the Insured Person is continuously covered without any break as defined under the applicable norms on Portability stipulated by IRDAI, then waiting period for the same would be reduced to the extent of prior coverage.
List of Specific disease/conditions/treatments:
I. Tumors, Cysts, polyps including breast lumps (benign) (Arbud, Granthi, including arbud in Sthana)
II. Polycystic ovarian disease (garbhashaya granthi),
Fibromyoma {Aartav dushti (Sowmya arbudham)},
Adenomyosis,
Endometriosis (Udavarthani yoni vyaazpt)
III. Prolapsed Uterus (Yoni bhramsha)
IV. Gout and Rheumatism (Vaathraktha and Aamvaat / Aadhya vata), Rheumatoid arthritis, Non-infective arthritis (Sandhi shool {Dhatukshay janya or Avrodhjanya, both, Sandhigata vata, Vata roga})
V. Ligament, Tendon or Meniscal tear (Sira, kandara, maamsgat vaat janya shool, sandhi shola)
VI. Prolapsed Inter-Vertebral Disc (Katishool, Greevashool, Grudhrasi vata) and Spinal Diseases including spondylitis/spondylosis unless arising from Accident
VII. Cholelithiasis (yakrut roga)
VIII. Pancreatitis
IX. Fissure/fistula in anus, haemorrhoids, pilonidal sinus (Arsha, Parikartika, bhagandar, gudagat vranshoth, nadi vrana)
X. Ulcer & erosion of stomach & duodenum
XI. Gastro Esophageal Reflux Disorder (GERD) (Parinamshool, annadravakhya shool, Amlapitta, Grahani)
XII. Liver Cirrhosis
XIII. Perineal Abscesses (bhagandhara)
XIV. Perianal / Anal Abscesses
XV. Calculus diseases of Urogenital system Example: Kidney stone, Urinary bladder stone (Ashmari of all types)
XVI. Benign Hyperplasia of prostate (Asththila vruddhi)
XVII. Varicocele (Vruddhi, Vrushanshoth)
XVIII. Cataract (avrana Shukla),
Retinal detachment,
Glaucoma (abhishyandha)
XIX. Congenital Internal Diseases
XX. Osteoarthritis and osteoporosis (Asthikshay/ asti gata vata)
XXI. Systemic connective tissue disorders, inflammatory polyarthropathies.
List of procedure/surgeries/treatments:
XXII. Adenoidectomy
XXIII. Mastoidectomy
XXIV. Tonsillectomy
XXV. Tympanoplasty
XXVI. Surgery for nasal septum deviation and
Nasal concha resection
XXVII. Surgery for Turbinate hypertrophy
XXVIII. Hysterectomy
XXIX. Joint replacement surgeries (for example: Knee replacement, Hip replacement)
XXX. Cholecystectomy
XXXI. Hernioplasty or Herniorraphy
XXXII. Surgery/procedure for Benign prostate enlargement
XXXIII. Surgery for Hydrocele/ Rectocele/Spermatocele
XXXIV. Surgery of varicose veins and varicose ulcers
XXXV. Obesity / Weight control procedures including Gastric bypass surgeries. (already covered in Code- Excl 06)
iii. 30 Days Waiting Period for all illnesses (Code- Excl 03):
(not applicable for accidents or on renewals)
a. Expenses related to the treatment of any Illness within 30 days from the first Policy commencement date shall be excluded except claims arising due to an Accident, provided the same are covered.
b. This exclusion shall not, however, apply if the Insured Person has Continuous Coverage for more than twelve months.
c. The within referred waiting period is made applicable to the enhanced Sum Insured in the event of granting higher Sum Insured subsequently.
B. Medical Exclusions ( 12 + (10 + 2) = 24)
i. Investigation and evaluation (Code- Excl 04):
a. Expenses related to any admission primarily for diagnostics and evaluation purposes only are excluded.
b. Any diagnostic expenses which are not related or not incidental to the current diagnosis and treatment are excluded.
ii. Rest cure, rehabilitation and respite care (Code- Excl 05):
a. Expenses related to any admission primarily for enforced bed rest and not for receiving treatment. This also includes:
i. Custodial care either at home or in a nursing facility for personal care such as help with activities of daily living such as bathing, dressing, moving around either by skilled nurses or assistant or non-skilled persons.
ii. Any services for people who are terminally ill to address physical, social, emotional and spiritual needs.
iii. Obesity/ Weight Control (Code- Excl 06):
Expenses related to surgical treatment of obesity that does not fulfil the below conditions:
a. Surgery to be conducted is upon the advice of the Doctor.
b. The Surgery/Procedure conducted should be supported by clinical protocols.
c. The member has to be 18 years of Age or older and
d. Body Mass Index (BMI);
i. greater than or equal to 40 or
ii. greater than or equal to 35 in conjunction with any of the following severe co-morbidities following failure of less invasive methods of weight loss:
1. Obesity-related cardiomyopathy
2. Coronary heart disease
3. Severe Sleep Apnea
4. Uncontrolled Type2 Diabetes
iv. Change-of-Gender treatments (Code- Excl07):
Expenses related to any treatment, including surgical management, to change characteristics of the body to those of the opposite sex.
v. Cosmetic or Plastic Surgery (Code- Excl 08):
Expenses for cosmetic or plastic Surgery or any treatment to change appearance unless for reconstruction following an Accident, Burn(s) or Cancer or as part of Medically Necessary Treatment to remove a direct and immediate health risk to the Insured Person. For this to be considered a medical necessity, it must be certified by the attending Medical Practitioner.
vi. Treatment for Alcoholism, drug or substance abuse or any addictive condition and consequences thereof (Code- Excl 12).
vii. Treatments received in health hydros, nature cure clinics, spas or similar establishments or private beds registered as a nursing home attached to such establishments or where admission is arranged wholly or partly for domestic reasons. (Code- Excl13)
viii. Dietary supplements and substances that can be purchased without prescription, including but not limited to Vitamins, minerals and organic substances unless prescribed by a Medical Practitioner as part of Hospitalization claim or day care procedure. (Code-Excl14)
ix. Refractive error (Code- Excl 15):
Expenses related to the treatment for correction of eye sight due to refractive error less than 7.5 dioptres.
x. Unproven treatments (Code- Excl 16):
Expenses related to any Unproven Treatment, services and supplies for or in connection with any treatment. Unproven treatments are treatments, procedures or supplies that lack significant medical documentation to support their effectiveness.
xi. Sterility and Infertility (Code- Excl 17):
Expenses related to Sterility and infertility. This includes:
i. Any type of contraception, sterilization
ii. Assisted Reproduction services including artificial insemination and advanced reproductive technologies such as IVF, ZIFT, GIFT, ICSI
iii. Gestational Surrogacy
iv. Reversal of sterilization
xii. Maternity (Code – Excl 18):
1. Medical treatment expenses traceable to childbirth (including complicated deliveries and caesarean sections incurred during Hospitalization) except ectopic pregnancy;
2. Expenses towards miscarriage (unless due to an Accident) and lawful medical termination of pregnancy during the Policy Period.
C. Non-Medical Exclusions (3 + 14 = 17)
i. Hazardous or Adventure Sports (Code- Excl 09):
Expenses related to any treatment necessitated due to participation as a professional in hazardous or adventure sports, including but not limited to, para-jumping, rock climbing, mountaineering, rafting, motor racing, horse racing or scuba diving, hand gliding, sky diving, deep-sea diving.
ii. Breach of law (Code- Excl 10):
Expenses for treatment directly arising from or consequent upon any Insured Person committing or attempting to commit a breach of law with criminal intent.
iii. Excluded Providers: (Code-Excl 11):
Expenses incurred towards treatment in any Hospital or by any Medical Practitioner or any other provider specifically excluded by the Insurer and disclosed in its website / notified to the Policyholders are not admissible. However, in case of life-threatening situations or following an Accident, expenses up to the stage of stabilization are payable but not the complete claim.
ii. Specific Exclusions (Exclusions other than as those mentioned under Section 3 (i) subsection A, B & C above)
We will neither be liable nor make any payment for any claim in respect of any Insured Person
which is caused by, arising from or in any way attributable to any of the following exclusions.
A. Medical Exclusions
i. Alcoholic pancreatitis or Alcoholic liver disease;
ii. Congenital External Diseases, defects or anomalies;
iii. Stem cell therapy; however, hematopoietic stem cells for bone marrow transplant for haematological conditions will be covered under this Policy,
iv. Growth Hormone Therapy;
v. Sleep-apnoea and Sleeping disorder;
vi. Admission primarily for administration (via any form or mode) of immunoglobulin infusion or supplementary medications like Zolendronic Acid, etc;
vii. Venereal disease, sexually transmitted disease or Illness;
viii. All preventive care including Health Check-ups, vaccination including inoculation and immunisations;
ix. Cost of dentures, dental implants and braces; Dental Treatment or Dental Surgery of any kind unless incidental to an admissible Hospitalization claim where the cause of admission is Accident;
x. Any form of Non-Allopathic treatment (except AYUSH Benefit), Hydrotherapy, Acupuncture, Reflexology, Chiropractic treatment or any other form of indigenous system of medicine.
xi. Any existing disease specifically mentioned as Permanent exclusion in the Policy Schedule.
xii. Non payable items as mentioned in Annexure I – List I of optional items available on Our website (www.tataaig.com) —as it is Add on
B. Non-Medical Exclusions
i. War or any act of war, invasion, act of foreign enemy, war like operations (whether war be declared or not) or caused during service in the armed forces of any country, civil war, public defence, rebellion, revolution, insurrection, military or usurped acts, nuclear weapons/materials, chemical and biological weapons, ionising radiation.
ii. Nuclear, chemical or biological attack or weapons, contributed to, caused by, resulting from or from any other cause or event contributing concurrently or in any other sequence to the loss, claim or expense. For the purpose of this exclusion: (irrelevant)
• Nuclear attack or weapons means the use of any nuclear weapon or device or waste or combustion of nuclear fuel or the emission, discharge, dispersal, release or escape of fissile/ fusion material emitting a level of radioactivity capable of causing any Illness, incapacitating disablement or death
• Chemical attack or weapons means the emission, discharge, dispersal, release or escape of any solid, liquid or gaseous chemical compound which, when suitably distributed, is capable of causing any Illness, incapacitating disablement or death.
• Biological attack or weapons means the emission, discharge, dispersal, release or escape of any pathogenic (disease producing) micro-organisms and/or biologically produced toxins (including genetically modified organisms and chemically synthesized toxins) which are capable of causing any Illness, incapacitating disablement or death.
iii. Any Insured Person’s participation or involvement in naval, military or air force operation.
iv. Intentional self-Injury or attempted suicide while sane or insane.
v. If the Insured Person is under the influence of intoxicating liquor or drugs or other intoxicants, except where the Insured Person is not directly responsible for the Injury/Accident though under influence of intoxication.
vi. Items of personal comfort and convenience like television (wherever specifically charged for), charges for access to telephone and telephone calls, internet, foodstuffs (except patient’s diet), cosmetics, hygiene articles, body care products and bath additive, barber or beauty service, guest service.
vii. Treatment rendered by a Medical Practitioner which is outside his discipline.
viii. Doctor’s fees charged by the Medical Practitioner sharing the same residence as an Insured Person or who is an immediate relative of an Insured Person’s family.
ix. Hearing aids, spectacles or contact lenses, etc. including optometric therapy.
x. Any treatment and associated expenses for alopecia, baldness, wigs or toupees, medical supplies including elastic stockings, diabetic test strips and similar products.
xi. Any treatment or part of a treatment that does not form part of ‘Reasonable and Customary charges’, nor is medically necessary;
xii. Expenses which are either not supported by a prescription of a Medical Practitioner or are not related to Illness or disease for which claim is admissible under the Policy.
xiii. Any external appliance and/or device used for diagnosis or treatment except when used intra-operatively. eg: Crutches
xiv. Any Illness diagnosed or Injury sustained or where there is change in health status of the member after date of proposal and before commencement of Policy and the same is not communicated and accepted by Us.
No Need to Know from here
Section 4 – General Terms and Clauses
i. Standard General Terms & Clauses
1. Disclosure of Information
The Policy shall be void and all premium paid thereon shall be forfeited to the Company in the event of established fraud, misrepresentation, misdescription or non-disclosure of any material fact by the policyholder.
(Explanation: “Material facts” for the purpose of this Policy shall mean all relevant information sought by the company in the proposal form and other connected documents to enable it to take informed decision in the context of underwriting the risk)
2. Condition Precedent to Admission of Liability
The terms and conditions of the Policy must be fulfilled by the Insured Person for the Company to make any payment for claim(s) arising under the Policy.
3. Claim Settlement (provision for Penal Interest)
i. The Company shall settle or reject a claim, as the case may be, within 15 days from the date of receipt of last necessary document.
ii. In the case of delay in the payment of a claim, the Company shall be liable to pay interest to the policyholder from the date of receipt of last necessary document to the date of payment of claim at a rate 2% above the bank rate.
iii. However, where the circumstances of a claim warrant an investigation in the opinion of the Company, it shall initiate and complete such investigation at the earliest, in any case not later than 30 days from the date of receipt of last necessary document. In such cases, the Company shall settle or reject the claim within 45 days from the date of receipt of last necessary document.
iv. In case of delay beyond stipulated 45 days, the Company shall be liable to pay interest to the policyholder at a rate 2% above the bank rate from the date of receipt of last necessary document to the date of payment of claim.
(Explanation: “Bank rate” shall mean the rate fixed by the Reserve Bank of India (RBl) at the beginning of the financial year in which claim has fallen due).
4. Complete Discharge
Any payment to the policyholder, Insured Person or his/ her nominees or his/ her legal representative or assignee or to the Hospital, as the case may be, for any benefit under the Policy shall be a valid discharge towards payment of claim by the Company to the extent of that amount for the particular claim.
5. Multiple Policies
i. In case of multiple policies taken by an Insured Person during a period from one or more insurers to indemnify treatment costs, the Insured Person shall have the right to require a settlement of his/her claim in terms of any of his/her policies. In all such cases the Insurer chosen by the Insured Person shall be obliged to settle the claim as long as the claim is within the limits of and according to the terms of the chosen Policy.
ii. Insured Person having multiple policies shall also have the right to prefer claims under this Policy for the amounts disallowed under any other Policy / policies even if the Sum Insured is not exhausted. Then the Insurer shall independently settle the claim subject to the terms and conditions of this Policy.
iii. If the amount to be claimed exceeds the Sum Insured under a single Policy, the Insured Person shall have the right to choose Insurer from whom he/she wants to claim the balance amount and We will assist the Insured Person in facilitating the same.
iv. Where an Insured Person has policies from more than one Insurer to cover the same risk on indemnity basis, the Insured Person shall only be indemnified the treatment costs in accordance with the terms and conditions of the chosen Policy.
6. Fraud
If any claim made by the Insured Person, is in any respect fraudulent, or if any false statement, or declaration is made or used in support thereof, or if any fraudulent means or devices are used by the Insured Person or anyone acting on his/her behalf to obtain any benefit under this Policy, all benefits under this Policy and the premium paid shall be forfeited.
Any amount already paid against claims made under this Policy but which are found fraudulent later shall be repaid by all recipient(s)/policyholder(s), who has made that particular claim, who shall be jointly and severally liable for such repayment to the Insurer.
For the purpose of this clause, the expression “fraud” means any of the following acts committed by the Insured Person or by his agent or the Hospital/doctor/any other party acting on behalf of the Insured Person, with intent to deceive the Insurer or to induce the Insurer to issue an insurance Policy:
a. the suggestion, as a fact of that which is not true and which the Insured Person does not believe to be true;
b. the active concealment of a fact by the Insured Person having knowledge or belief of the fact;
c. any other act fitted to deceive; and
d. any such act or omission as the law specially declares to be fraudulent.
The Company shall not repudiate the claim and / or forfeit the Policy benefits on the ground of Fraud, if the Insured Person / beneficiary can prove that the misstatement was true to the best of his knowledge and there was no deliberate intention to suppress the fact or that such misstatement of or suppression of material fact are within the knowledge of the Insurer.
7. Cancellation
The policyholder may cancel this Policy by giving 7 days written notice and in such an event, the Company shall refund proportionate premium for unexpired Policy Period. No refunds of premium shall be made in respect of Cancellation where any claim has been admitted or has been lodged or any benefit under this Policy has been availed by the Insured Person.
The Company may cancel the Policy at any time on grounds of established fraud, misrepresentation or non-disclosure of material facts by the Policyholder/ Insured Person by giving 15 days’ written notice. There would be no refund of premium on cancellation on grounds of established fraud, misrepresentation, non-disclosure of material facts.
8. Migration
The Insured Person will have the option to migrate the Policy to other health insurance products/plans offered by the company by applying for Migration of the Policy at least 30 days before the Policy Renewal date per IRDAI guidelines. lf such person is presently covered and has been continuously covered without any lapses under any health insurance product/plan offered by the company, the Insured Person will get the accrued continuity benefits to the extent of the Sum Insured, No Claim Bonus, Specific Waiting periods, waiting period for pre-existing diseases, Moratorium period etc. in the previous policy to the migrated policy, as applicable.
For Detailed Guidelines on Migration, kindly refer
Insurance Regulatory and Development Authority of India (Insurance Products) Regulations, 2024 F. No. IRDAI/Reg/8/202/2024 dated 20th March, 2024 and Master Circular on IRDAI (Insurance Products) Regulations 2024- Health Insurance Ref: IRDAI/HLT/CIR/PRO/84/5/ 2024 dated 29th May 2024 and subsequent amendments thereof.
9. Portability
The Insured Person will have the option to port the Policy to other insurers by applying to such Insurer to port the entire Policy along with all the members of the family, if any, at least 30 days before, but not earlier than 60 days from the Policy Renewal date per IRDAI guidelines. If such person is presently covered and has been continuously covered without any lapses under any health insurance Policy with an Indian General/Health Insurer, the proposed Insured Person will get the accrued continuity benefits to the extent of the Sum Insured, No Claim Bonus, specific waiting periods, waiting period for pre-existing disease, Moratorium period etc from the existing Insurer to the acquiring Insurer in the previous policy, as applicable.
For Detailed Guidelines on Portability, kindly refer
Insurance Regulatory and Development Authority of India (Insurance Products) Regulations, 2024 F. No. IRDAI/Reg/8/202/2024 dated 20th March, 2024 and Master Circular on IRDAI (Insurance Products) Regulations 2024- Health Insurance Ref: IRDAI/HLT/CIR/PRO/84/5/ 2024 dated 29th May 2024 and their subsequent amendments thereof.
Requirement:
- Completed proposal form,
- Supporting Medical papers (wherever applicable),
- Previous policy copies, IRDAI portability form (as applicable)
10. Renewal of Policy
The Policy shall ordinarily be renewable except on grounds of established fraud, non-disclosure or misrepresentation by the Insured Person.
i. Renewal shall not be denied on the ground that the Insured Person had made a claim or claims in the preceding Policy Years.
ii. Request for Renewal along with requisite premium shall be received by the Company before the end of the Policy Period.
iii. Single premium payment mode Policy can be renewed within the Grace Period of 30 days to maintain continuity of benefits without Break in Policy. Coverage is not available during the Grace Period after the end of the Policy Period. If not renewed under the Grace Period, the Policy shall terminate at the end of the Grace Period.
iv. The Grace Period for payment of the premium during the Policy Period, for instalment premium shall be fifteen days where premium payment mode is monthly and thirty days in all other cases (Annual/ Half-Yearly/ Quarterly/Limited Premium paying term).
v. Coverage during such Grace Period (in case of instalment premium):
a. Within the Policy Period – coverage will be available from the due date of instalment premium till the date of receipt of premium by Company within the Grace Period.
b. At the end of the Policy Period – the Policy shall terminate and can be renewed within the Grace Period of 30 days to maintain continuity of benefits without Break in Policy. Coverage is not available during the Grace Period after the end of the Policy Period.
vi. The Insured Person will get the accrued continuity benefit to the extent of Sum Insured, No Claim Bonus, Specified Waiting Periods, waiting periods for pre-existing diseases, Moratorium period, as applicable, in the event of payment of premium within the stipulated Grace Period.
vii. No loading shall apply on Renewals based on individual claims experience.
11. Withdrawal of Policy
i. In the likelihood of this product being withdrawn in future, the Company will intimate the Insured Person about the same 90 days prior to expiry of the Policy.
ii. Insured Person will have the option to migrate to similar health insurance product available with the Company at the time of Renewal with all the accrued continuity benefits such as No Claim Bonus, waiver of waiting period as per IRDAI guidelines, provided the Policy has been maintained without a break.
12. Moratorium Period
After completion of five continuous years of coverage (including Portability and Migration) in health insurance Policy, no Policy and claim shall be contestable by the Insurer on grounds of non- disclosure, misrepresentation, except on grounds of established fraud. This continuous period of five years is called as moratorium period. The moratorium would be applicable for the sums insured of the first Policy. Wherever the Sum Insured is enhanced, completion of five continuous years would be applicable from the date of enhancement of sums insured only on the enhanced limits. The policies would however be subject to all limits, sub limits, Co-Payments, Aggregate Deductibles (If opted) as per the Policy contract.
13. Possibility of Revision of Terms of the Policy Including the Premium Rates
The Company may revise or modify the terms of the Policy including the premium rates. The Insured Person shall be notified three months before the changes are effected.
14. Free look period
The insured person shall be provided a free look period of thirty days beginning from the date of receipt of the policy document, whether received electronically or otherwise, to review the terms and conditions of the policy, and to return the same if not acceptable.
If the Insured Person has not made any claim during the Free Look Period, the Insured Person shall be entitled to a refund of the premium paid subject to deduction of proportionate risk premium for the period of cover and the expenses, if any, incurred by Us on medical examination of the proposer and stamp duty charges.
15. Redressal of Grievance
At TATA AIG, We strive to provide the best service to Our customers. If You’re not satisfied and wish to lodge a complaint, please call Our 24/7 toll-free number 1800-266-7780 /1800 22 9966 (For Senior Citizen) or 022-66939500 (toll charges apply), or email Us at customersupport@tataaig.com. We will investigate and respond within the regulatory turnaround time (TAT).
Escalation Level 1
If You do not receive a response or are not satisfied with the resolution, please contact Us at manager.customersupport@tataaig.com.
Escalation Level 2
If You still need assistance, reach out to the Head of Customer Services at head.customerservices@tataaig.com. We will provide Our final response within the regulatory TAT.
If You’re still not satisfied after this process, You may approach the Insurance Ombudsman of concerned jurisdiction.
You can also lodge a grievance on the Bima Bharosa Grievance Redressal Portal: https://bimabharosa.irdai.gov. in
The name and address of the Insurance Ombudsman of competent jurisdiction is provided under Annexure A of this Policy.
16. Nomination
The policyholder is required at the inception of the Policy to make a nomination for the purpose of payment of claims under the Policy in the event of death of the policyholder. Any change of nomination shall be communicated to the company in writing and such change shall be effective only when an endorsement on the Policy is made. In the event of death of the policyholder, the Company will pay the nominee {as named in the Policy Schedule/Endorsement (if any)} and in case there is no subsisting nominee, to the legal heirs or legal representatives of the policyholder whose discharge shall be treated as full and final discharge of its liability under the Policy.
ii. Specific terms and clauses (terms and clauses other than those mentioned under Section 4 (i) above)
17. Insured Person
i. Only those persons named as an Insured Person in the Schedule shall be covered under this Policy.
ii. Any eligible person may be added during the Policy Period after his proposal has been accepted by Us, additional premium has been paid and We have issued an endorsement confirming the addition of such person as an Insured Person.
18. Loadings
i. We may apply a risk loading on the premium payable (based upon the declarations made in the proposal and the health status of the persons proposed for insurance).
ii. The loading shall be applied basis outcome of Our underwriting.
iii. These loadings are applied from Commencement Date of the Policy including subsequent Renewal(s) with Us and on the applicable Sum Insured for each Policy Year including increased Sum Insured, if any.
a. We will inform You about the applicable risk loading through a counter offer letter.
b. You need to revert to Us with consent and additional premium (if any), within 15 days of the issuance of such counter offer letter.
c. In case, You neither accept the counter offer nor revert to Us within 15 days, We shall cancel Your application and refund/ release the amount subject to deduction of the Pre-Policy Check up charges, as applicable.
iv. Please note that We will issue Policy only after getting Your consent.
19. Entire Contract
i. This Policy, its Schedule, endorsement(s), proposal constitutes the entire contract of insurance. No change in this Policy shall be valid unless approved by Us and such approval be endorsed hereon.
ii. This Policy and the Schedule shall be read together as one contract and any word or expression to which a specific meaning has been attached in any part of this Policy or of the Schedule shall bear such meaning wherever it may appear.
20. Notices
i. Any notice, direction or instruction under this Policy shall be in writing and if it is to:
a. Any Insured Person, then it shall be sent to You at Your address specified in the Schedule to this Policy and You shall act for all Insured Persons for these purposes.
b. Us, it shall be delivered to Our address specified in the Schedule to this Policy. No insurance agents, brokers or other person or entity is authorised to receive any notice, direction or instruction on Our behalf unless We have expressly stated to the contrary in writing.
21. Premium Payment Zone
For the purpose of premium computation, the country is divided into three Zones {as mentioned in Section 1: ii. Specific Definitions. 15. Zone(s)} and the premium payable under this Policy will be computed based on the residential location/address as provided by the proposer/Insured Person in the proposal form.
Here ‘Address’ implies the place where the person ordinarily resides. In case proposed prospect(s) reside at multiple addresses, then address of the person residing in the highest Zone will be considered.
Premium Rates:
a. The premium will be charged on the completed age of the Insured Person.
b. Premium rates are subject to change.
c. The premium for the policy will remain the same for the policy period as mentioned in the policy schedule.
d. For family floater, premium is calculated by adding the premium of respective individual members and applying family floater discount.
e. Monthly/Quarterly/Half-Yearly/Annual and Limited Premium paying term instalment option would be allowed and following loadings shall be applicable as per the selected instalment option and Policy Tenure:
| Loading % | |||
| Instalment Option/Tenure | 1 Year Policy | 2 Year Policy | 3 Year Policy |
| Monthly | 5.00% | 9.00% | 13.00% |
| Quarterly | 4.00% | 8.00% | 12.00% |
| Half-Yearly | 2.50% | 7.00% | 11.00% |
Limited Premium paying term:
| EMI Tenure / Policy Tenure | Loading % | ||
| 1 Year | 2 Year | 3 Year | |
| 2 Months | 0.50% | 0.50% | 0.50% |
| 3 Months | 1.25% | 1.25% | 1.25% |
| 6 Months | 2.50% | 2.50% | 2.50% |
| 12 Months | 5.00% | 5.00% | 5.00% |
If the insured person has opted for Payment of Premium on an instalment basis as mentioned in the policy Schedule, the following Conditions shall apply (notwithstanding any terms contrary elsewhere in the policy)
I. Grace Period of 15 days would be given to pay the installment premium due for the policy where premium payment mode is monthly and 30 days in all other cases (Annual/Half-Yearly/ Quarterly/ Limited Premium paying term) during the policy period. During such grace period, coverage shall be available from the due date of installment premium till the date of receipt of premium by Company.
II. The insured person will get the accrued continuity benefit in respect of the Waiting Periods, Specific Waiting Periods in the event of payment of premium within the stipulated grace Period.
III. No interest will be charged lf the installment premium is not paid on due date
IV. In case of installment premium due not received within the grace period, the policy will get cancelled. In such scenario, in case of Limited Premium paying term mode, premium will be refunded on pro rata basis after deducting administrative costs (if any), subject to no claims under the Policy.
V. In the event of a claim, all subsequent premium instalments shall immediately become due and payable.
VI. The company has the right to recover and deduct all the pending installments from the claim amount due under the policy.
For premium rates, kindly visit our
22. Premium Refund in case of demise of the Insured Person
The coverage for the Insured Person(s) shall automatically terminate in case of his/ her (Insured Person) demise. However, the cover shall continue for the remaining Insured Persons till the end of Policy Period.
Provided no claim has been made and deletion from Policy takes place on account of death of the Insured Person during the Policy Period, pro-rata refund of premium of the deceased Insured Person for the balance period of the Policy will be made. Refund will be made to the Policy holder or the nominee as the case may be in case of demise of the Policy holder. We would require death certificate of the Deceased Insured Person for processing of the refund amount.
The other Insured Persons may also apply to renew the Policy. In the event of change of Proposer, all relevant particulars in respect of such person (including his/her relationship with the Insured Person) must be submitted to the company along with the application.
Section 5 – Claims Procedure and Claims Payment
This section explains about the procedure involved to file a valid claim by the Insured Person and processes related to assessment, cost sharing and management of the claim. All the procedures and processes such as Notification of Claim, availing cashless service, supporting claim documents and related claim terms of payment are explained in this section.
a. Notification of Claim / Intimation & Assistance:
Every claim needs to be notified to Us either in writing or email or through a call to Our tollfree number, as mentioned in the Policy Schedule, within the stipulated timelines as mentioned below.
| S.No. | Event | We or Our TPA* must be informed: |
| 1 | If any treatment for which a claim may be made and that treatment requires planned Hospitalization/ Day Care Treatment/ AYUSH/ Domiciliary Treatment: | At least 48 hours prior to the Insured Person’s admission/ start of treatment. |
| 2 | If any treatment for which a claim may be made and that treatment requires emergency Hospitalization/ Day Care Treatment | Within 24 hours of the Insured Person’s admission to Hospital or at the time of discharge, whichever is earlier. |
*TPA as mentioned in the Policy Schedule, if applicable.
Timely intimation of claim in Our prescribed format is a pre-condition for admission of liability.
We may waive off this condition in extreme cases of hardship where it is proved to Our satisfaction that under the circumstances in which You were placed, it was not possible for You or any other person to give notice or file claim within the prescribed time limit.
Claim Related Information:
For any claim related query, intimation of claim and submission of claim related documents, You can contact us through:
| Claims Servicing Details | |
| Name | TAGIC Health Claims |
| Claims Administrator Address | TATA AIG General Insurance Company Limited, 5th and 6th Floor, Imperial Towers, H.No 7-1-6-617/A, GHMC No – 615,616, Ameerpet, Hyderabad – 500016, Telangana, Phone: 040-66864900 |
| Email ID | healthclaimsupport@tataaig.com |
| Toll-Free No.: | 1800 266 7780 or 1800 229 966 (For Senior Citizens) |
| Website | www.tataaig.com |
b. Cashless Service
| Treatment, Consultation or Procedure: | Taken at: | Cashless Service is Available: | We must be given notice that the Insured Person wishes to avail cashless service accompanied by full particulars: |
| If any planned treatment, consultation or procedure for which a claim may be made: | Network Provider | We will provide cashless service by making payment to the extent of Our liability directly to the Network Hospital. | At least 48 hours before the planned Hospitalization |
| If any treatment, consultation or procedure for which a claim may be made, requiring emergency Hospitalization | Network Provider | We will provide cashless service by making payment to the extent of Our liability directly to the Network Hospital. | Within 24 hours of the Hospitalization and prior to discharge |
c. Procedure for Cashless Service
i. Cashless Service is only available at Our Network Provider.
Please refer to our website(www.tataaig.com) or call us on our toll free number at <<1800-266- 7780>> for empaneled hospital list.
ii. In order to avail cashless treatment, the following procedure must be followed by You:
a. Prior to taking treatment and/or incurring Medical Expenses at a Network Provider, You must notify Our designated TPA/Us and request pre-authorization.
b. Our designated TPA/We will check Your coverage as per the eligibility and send an authorization letter to the provider. You have to provide the ID card issued to You along with any other information or documentation that is requested by the TPA/Us to the Network Provider.
c. In case of deficiency in the documents sent to TPA/Us for cashless authorization or the ailment /treatment is not covered under the Policy, the same shall be communicated to the Hospital/You by TPA/Us.
d. We/TPA will respond within turn around time as prescribed by the Regulator under the Master Circular on IRDAI (Insurance Products) Regulations 2024- Health Insurance Ref: IRDAI/HLT/CIR/PRO/84/5/ 2024 and its subsequent amendments thereof.
e. Rejection of cashless in no way indicates rejection of the claim. You are required to submit the claim along with required documents for Us to decide on the admissibility of the claim.
f. If the cashless is approved, the original bills and evidence of treatment in respect of the same shall be left with the Network Provider.
g. Pre-authorization does not guarantee that all costs and expenses will be covered. We reserve the right to review each claim for Medical Expenses and accordingly coverage will be determined according to the terms and conditions of this Policy.
Procedure for reimbursement claims:
• Our TPA/We must be informed within 7 days of completion of such treatment, consultation or procedure using the Claim Intimation Form.
• Please send the duly signed claim form and all the information/documents mentioned therein to our TPA/Us within 15 days of the occurrence of the Incident.
• Please refer to claim form for complete documentation.
• If there is any deficiency in the documents/information submitted by you, our TPA/We will send the deficiency letter within 7 working days of receipt of the claim documents.
• On receipt of the complete set of claim documents, We will send the payment for the admissible amount, along with a settlement statement within 15 days.
• The payment will be sent in the name of the proposer/ Nominee(s) in case of death of Proposer.
Kindly send the claim documents to:
TATA AIG General Insurance Co. Ltd. 5th and 6th Floor, Imperial Towers, H.No 7-1-6-617/A, GHMC No-615, 616, Ameerpet, Hyderabad – 500016, Telangana, Phone-040- 66864900.
Turn Around Time (TAT) for claims settlement:
TAT for preauthorization of cashless facility and for cashless final bill authorization shall be as prescribed by the Regulator under the Master Circular on IRDAI (Insurance Products) Regulations 2024- Health Insurance Ref: IRDAI/HLT/CIR/PRO/84/5/ 2024 and its subsequent amendments thereof.
Assistance:
- Please refer to our website www.tataaig.com or call us on our toll free number at <1800-266-7780> to get details on our empanelled hospitals and list of Excluded providers/ Blacklisted Hospitals.
- Helpline number: Toll Free: 1800 266 7780 or 1800 22 9966 (only for Senior Citizen policyholders)
- Please refer our website www.tataaig.com to download claim form.
d. Supporting Documentation & Examination
i. We or Our TPA may require documentation, medical records and information to establish the circumstances of the claim, its quantum or Our liability for the claim within 15 days or earlier of Our request or the Insured Person’s discharge from Hospitalization or completion of treatment.
ii. In case the delay is at Your end, failure to furnish such evidence within the time required shall not invalidate nor reduce any claim if You can satisfy Us that it was not reasonably possible for You to give proof within such time.
iii. We may accept claims where documents have been provided after a delayed interval only in special circumstances and for the reasons beyond the control of the Insured Person.
iv. Such documentation will include the following:
a. Our claim form, duly completed and signed for on behalf of the Insured Person. We, upon receipt of a notice of claim, will furnish Your representative with such forms as We may require for filing proofs of loss or You may download the claim form from Our Web site.
b. Original Bills (pharmacy purchase bill, consultation bill, diagnostic bill, medical devices) and any attachments thereto like receipts or prescriptions in support of any amount claimed which will then become Our property.
c. All medical reports, case histories, investigation reports, indoor case papers/ treatment papers (in reimbursement cases, if available), discharge summaries.
d. A precise diagnosis of the treatment for which a claim is made.
e. A detailed list of the individual medical services and treatments provided and a unit price for each in case not available in the submitted Hospital bill.
f. Prescriptions that name the Insured Person and in the case of drugs: the drugs prescribed, their price and a receipt for payment. In case of pre/post Hospitalization claim Prescriptions must be submitted with the corresponding Doctor/Hospital invoice.
g. All pre and post investigation, treatment and follow up (consultation) records pertaining to the present ailment for which claim is being made, if and where applicable.
h. Treating doctor’s certificate regarding missing information in case histories e.g. Circumstance of Injury and Alcohol or drug influence at the time of Accident, if available.
i. Copy of settlement letter from other insurance company or TPA.
j. Stickers and invoice of implants used during Surgery.
k. Copy of MLC (Medico legal case) records, if carried out and FIR (First information report), if registered, in case of claims arising out of an Accident and available with the claimant.
l. Regulatory requirements as amended from time to time, currently mandatory NEFT (to enable direct credit of claim amount in bank account) and KYC (recent ID/Address proof and photograph) requirements.
m. Legal heir/succession certificate, if required
n. PM report (wherever applicable)
o. The Company reserves the right to call for additional documents wherever required.
v. Note: In case You are claiming for the same event under an indemnity-based Policy with Us and with another Insurer and are required to submit the original documents related to Your treatment with that particular Insurer, then We will require the attested copies of such documents along with a declaration from the particular Insurer specifying the availability of the original copies of the specified treatment documents with it.
vi. We at Our own expense, shall have the right and opportunity to examine Insured Persons through Our Authorised Medical Practitioner whose details will be notified to Insured Person when and as often as We may reasonably require during the pendency of a claim hereunder.
e. Claims Assessment and Payment
i. General
a. We shall be under no obligation to make any payment under this Policy unless:
– We have received all premium payments in full and in time and
– We have been provided with the documentation and information which We or Our TPA has requested to establish the circumstances of the claim, its quantum or Our liability for it, and
– unless You have complied with Your obligations under this Policy.
b. This Policy only covers claims incurred within India, and payments under this Policy shall only be made in Indian Rupees within India.
c. Medical Expenses incurred for AYUSH Treatment shall be assessed only under benefit B7 of this Policy and shall be admissible only if incurred within India.
Where an ailment/ Illness/ disease is excluded under both exclusions with waiting Periods (as specified under Section 3 (i) Sub section (A) and under any other Policy exclusion, then for assessment of liability, any expense related to that ailment/ Illness/ disease shall not be covered under this Policy.
Claim assessment for policies with instalment Premium Payment Mode:
In the event of a claim, all subsequent premium instalments shall immediately become due and payable.
ii. Sequence of applicability & Utilization
a. The sequence of assessment of claim shall be as per table given below:
| Steps | Assessment | Applicability |
| 1 | Amount of Claim Intimated | √ |
| 2 | Less Non-Payable expenses# | √ |
| 3 | =Admissible Expenses | √ |
| 4 | Less Associated Medical Expenses as defined under the Policy (if applicable) | √ |
| 5 | =Final Assessed Amount | √ |
| 6 | Less Aggregate Deductible (if Opted)* | If applicable |
| 7 | =Final Assessed Liability | √ |
| Claim Payable subject to applicable Balance Sum Insured (including accrued Cumulative Bonus)/ Benefit Limit | ||
# Deduction may vary subject to selection of ‘Consumables Benefit’ optional cover.
* Aggregate Deductible, if opted, shall be applicable on aggregate of all claims as assessed under the final assessed amount for a given Policy Year.
The payment of any claim under this Policy shall be subject to Aggregate Deductible (if opted), benefit limits, balance Sum Insured and accrued Cumulative Bonus, if available.
b. The sequence of utilization of benefit for a claim shall be in the following order if applicable and available:
1. Balance Sum Insured/Early Access (if opted),
2. Any accrued Cumulative Bonus,
3. Restore Infinity Plus amount/Infinite Advantage amount (If opted)
Supporting Documentation & Examination
Insured Person or someone booking services on Your behalf shall provide Us with identification documentation, medical records and information We may request to establish the circumstances of the claim.
Your claim will be processed including cashless and final bill authorization as prescribed by the Regulator under the Master Circular on IRDAI (Insurance Products) Regulations 2024- Health Insurance Ref: IRDAI/HLT/CIR/PRO/84/5/ 2024 and its subsequent amendments thereof.
Section 6 – Dispute Resolution
Any and all disputes or differences under or in relation to this Policy shall be determined by the Indian Courts and subject to Indian law.
Annexure A
NAMES OF OMBUDSMAN AND ADDRESSES OF OMBUDSMAN CENTRES
| Sr.No. | Centre | Address & Contact | Jurisdiction of Office Union Territory, District |
| 1 | AHMEDABAD | Office of the Insurance Ombudsman, Jeevan Prakash Building, 6th floor, Tilak Marg, Relief Road, AHMEDABAD – 380 001. Tel.: 079 – 25501201/02 Email: bimalokpal.ahmedabad@cioins.co.in | Gujarat, Dadra & Nagar Haveli, Daman and Diu |
| 2 | BENGALURU | Office of the Insurance Ombudsman, Jeevan Soudha Building,PID No. 57-27- N-19 Ground Floor, 19/19, 24th Main Road, JP Nagar, Ist Phase, Bengaluru – 560 078. Tel.: 080 – 26652048 / 26652049 Email: bimalokpal.bengaluru@cioins.co.in | Karnataka |
| 3 | BHOPAL | Office of the Insurance Ombudsman, 1st floor,”Jeevan Shikha”, 60-B,Hoshangabad Road, Opp. Gayatri Mandir,Arera Hills Bhopal – 462 011. Tel.: 0755 – 2769201 / 2769202/ 2769203 Email: bimalokpal.bhopal@cioins.co.in | Madhya Pradesh, Chhattisgarh |
| 4 | BHUBHANESHWAR | Office of the Insurance Ombudsman, 62, Forest park, Bhubaneswar – 751 009. Tel.: 0674 – 2596461 /2596455/ 2596429/ 2596003 Email: bimalokpal.bhubaneswar@cioins.co.in | Odisha |
| 5 | CHANDIGARH | Office Of The Insurance Ombudsman, Jeevan Deep Building SCO 20-27, Ground Floor Sector- 17 A, Chandigarh – 160 017. Tel.: 0172 – 2706468 Email: bimalokpal.chandigarh@cioins.co.in | Punjab, Haryana (excluding Gurugram, Faridabad, Sonepat and Bahadurgarh), Himachal Pradesh, Union Territories of Jammu & Kashmir, Ladakh & Chandigarh. |
| 6 | CHENNAI | Office of the Insurance Ombudsman, Fatima Akhtar Court, 4th Floor, 453, Anna Salai, Teynampet, CHENNAI – 600 018. Tel.: 044 – 24333668 / 24333678 Email: bimalokpal.chennai@cioins.co.in | Tamil Nadu, Puducherry Town and Karaikal (which are part of Puducherry) |
| 7 | DELHI | Office of the Insurance Ombudsman, 2/2 A, Universal Insurance Building, Asaf Ali Road, New Delhi – 110 002. Tel.: 011 – 46013992/ 23213504/ 23232481 Email: bimalokpal.delhi@cioins.co.in | Delhi & following Districts of Haryana – Gurugram, Faridabad, Sonepat & Bahadurgarh |
| 8 | GUWAHATI | Office of the Insurance Ombudsman, Jeevan Nivesh, 5th Floor, Near Panbazar, S.S. Road, Guwahati – 781001(ASSAM). Tel.: 0361 – 2632204 / 2602205/ 2631307 Email: bimalokpal.guwahati@cioins.co.in | Assam, Meghalaya, Manipur, Mizoram, Arunachal Pradesh, Nagaland and Tripura |
| 9 | HYDERABAD | Office of the Insurance Ombudsman, 6-2-46, 1st floor, “Moin Court”, Lane Opp. Hyundai Showroom, A. C. Guards, Lakdi-Ka-Pool, Hyderabad – 500 004. Tel.: 040 – 23376991 / 23376599 / 23328709 / 23325325 Email: bimalokpal.hyderabad@cioins.co.in | Andhra Pradesh, Telangana, Yanam and part of Union Territory of Puducherry |
| 10 | JAIPUR | Office of the Insurance Ombudsman, Jeevan Nidhi – II Bldg., Gr. Floor, Bhawani Singh Marg, Jaipur – 302 005. Tel.: 0141- 2740363 Email: bimalokpal.jaipur@cioins.co.in | Rajasthan |
| 11 | KOCHI | Office of the Insurance Ombudsman, 10th Floor, Jeevan Prakash, LIC Building, Opp to Maharaja’s College Ground, M.G.Road, Kochi – 682 011. Tel.: 0484 – 2358759 Email: bimalokpal.ernakulam@cioins.co.in | Kerala, Lakshadweep, Mahe-a part of Union Territory of Puducherry |
| 12 | KOLKATA | Office of the Insurance Ombudsman, Hindustan Bldg. Annexe, 7th Floor, 4, C.R. Avenue, KOLKATA – 700 072. Tel.: 033 – 22124339 / 22124341 Email: bimalokpal.kolkata@cioins.co.in | West Bengal, Sikkim, Andaman & Nicobar Islands |
| 13 | LUCKNOW | Office of the Insurance Ombudsman, 6th Floor, Jeevan Bhawan, Phase-II, Nawal Kishore Road, Hazratganj, Lucknow – 226 001. Tel.: 0522 – 4002082 / 3500613 Email: bimalokpal.lucknow@cioins.co.in | Districts of Uttar Pradesh : Lalitpur, Jhansi, Mahoba, Hamirpur, Banda, Chitrakoot, Allahabad, Mirzapur, Sonbhabdra, Fatehpur, Pratapgarh, Jaunpur,Varanasi, Gazipur, Jalaun, Kanpur, Lucknow, Unnao, Sitapur, Lakhimpur, Bahraich, Barabanki, Raebareli, Sravasti, Gonda, Faizabad, Amethi, Kaushambi, Balrampur, |
| Basti, Ambedkarnagar, Sultanpur, Maharajgang, Santkabirnagar, Azamgarh, Kushinagar, Gorkhpur, Deoria, Mau, Ghazipur, Chandauli, Ballia, Sidharathnagar | |||
| 14 | MUMBAI | Office of the Insurance Ombudsman, 3rd Floor, Jeevan Seva Annexe, S. V. Road, Santacruz (W), Mumbai – 400 054. Tel.: 022 – 69038800/27/29/31/32/33 Email: bimalokpal.mumbai@cioins.co.in | List of wards under Mumbai Metropolitan Region excluding wards in Mumbai – i.e M/E, M/W, N , S and T covered under Office of Insurance Ombudsman Thane and areas of Navi Mumbai. |
| 15 | NOIDA | Office of the Insurance Ombudsman, Bhagwan Sahai Palace 4th Floor, Main Road, Naya Bans, Sector 15, Distt: Gautam Buddh Nagar, U.P- 201301. Tel.: 0120-2514252 / 2514253 Email: bimalokpal.noida@cioins.co.in | State of Uttarakhand and the following Districts of Uttar Pradesh: Agra, Aligarh, Bagpat, Bareilly, Bijnor, Budaun, Bulandshehar, Etah, Kannauj, Mainpuri, Mathura, Meerut, Moradabad, Muzaffarnagar, Oraiyya, Pilibhit, Etawah, Farrukhabad, Firozbad, Gautam Buddh nagar, Ghaziabad, Hardoi, Shahjahanpur, Hapur, Shamli, Rampur, Kashganj, Sambhal, Amroha, Hathras, Kanshiramnagar, Saharanpur. |
| 16 | PATNA | Office of the Insurance Ombudsman, 2nd Floor, Lalit Bhawan, Bailey Road, Patna 800 001. Tel.: 0612-2547068 Email: bimalokpal.patna@cioins.co.in | Bihar, Jharkhand |
| 17 | PUNE | Office of the Insurance Ombudsman, Jeevan Darshan Bldg., 3rd Floor, C.T.S. No.s. 195 to 198, N.C. Kelkar Road, Narayan Peth, Pune – 411 030. Tel.: 020-24471175 Email: bimalokpal.pune@cioins.co.in | State of Goa and State of Maharashtra excluding areas of Navi Mumbai, Thane district, Palghar District, Raigad district & Mumbai Metropolitan Region |
| 18 | THANE | Office of the Insurance Ombudsman, 2nd Floor, Jeevan Chintamani Building, Vasantrao Naik Mahamarg, Thane (West) Thane – 400604 Email: bimalokpal.thane@cioins.co.in | Area of Navi Mumbai, Thane District, Raigad District, Palghar District and wards of Mumbai, M/East, M/West, N, S and T.” |
For updated list and details of Insurance Ombudsman Offices, please visit website https://www.cioins.co.in/Ombudsman
Section 64VB of the Insurance Act, 1938 – Commencement of risk cover under the Policy is subject to receipt of premium by Tata AIG General Insurance Company Limited.
Prohibition of Rebates – Section 41 of the Insurance Act, 1938 as amended by Insurance Laws (Amendment) Act, 2015.
1. No person shall allow or offer to allow, either directly or indirectly, as an inducement to any person to take out or renew or continue an insurance in respect of any kind of risk relating to lives or property in India, any rebate of the whole or part of the commission payable or any rebate of the premium shown on the Policy, nor shall any person taking out or renewing or continuing a Policy accept any rebate, except such rebate as may be allowed in accordance with the published prospectuses or tables of the Insurer.
2. Any person making default in complying with the provisions of this section shall be liable for a penalty which may extend to ten lakh rupees.
“Insurance is a subject matter of solicitation”. For more details on risk factors, terms and conditions,
please read Policy document carefully before concluding a sale.
Benefit Table:
| Benefit Name | Coverage Limit |
| Sum Insured options (in ) | 5 / 7.5 / 10 / 15 / 20 / 25 / 50 / 75 / 100 / 200 / 300 Lakh |
| In-Patient Treatment | Up to Sum Insured |
| Pre-Hospitalization expenses | 90 Days, Upto Sum Insured |
| Post-Hospitalization expenses | 90 Days, Upto Sum Insured |
| Day Care Procedures | All Day Care Treatments, Upto Sum Insured |
| Organ Donor | Up to Sum Insured |
| Domiciliary Treatment | Up to Sum Insured |
| AYUSH Benefit | Upto Sum Insured |
| Ambulance Cover | Up to Sum Insured |
| Restore Infinity Plus | Unlimited restorations during a policy year |
| Daily Cash for choosing Twin Sharing Accommodation | Rs 1200 per day (Over & Above base sum insured) Available if the room category eligibility is ‘Single Private Room’ or higher than the Single Private Room |
| Daily Cash for choosing Multi-Sharing Accommodation | Rs 1500 per day (Over & Above base sum insured) Available if the room category eligibility is ‘Single Private Room’ or higher than the Single Private Room |
| No Claim Bonus | For every claim free policy year: Cumulative Bonus: 50% of the base Sum Insured of the expiring Policy, maximum upto 100% (50% decrease in subsequent policy year, in case of claim). OR 1% Discount in Renewal Premium Cumulative Bonus applies only if Discount in Renewal Premium is not availed. |
| Room Category** | Single Private Room |
| Optional Covers | |
| Consumables Benefit | NME- Non-Medical Expenses (specified consumables) covered Up to Sum Insured |
| Maternity Care | 10% of Sum Insured, maximum up to Rs. 1,00,000 per policy year (Over & Above base sum insured) |
| Reduction of Maternity Care Waiting Period | Reduction of ‘Maternity Care’ waiting period to 1 year |
| Infinite Advantage | Payment of any one claim during the lifetime of the Policy, without any limits |
| Early Access | For single premium multi-year policies, the Sum Insured of the policy period shall be available for utilization anytime during the Policy Period for admissible claim(s) |
| Room Category Select** | Any Room/ Twin sharing Accommodation |
| Aggregate Deductible | Deductible options (Rs.): 10,000/ 25,000/ 50,000/ 1,00,000 |
| Suitability | |
| Entry Age | No minimum/ maximum entry age limit |
| Policy Term | 1 Year/ 2 Years/ 3 Years (with lifetime renewal) |
| Coverage Options & Relationships | Family Floater: Self, spouse and up to 3 dependent children, up to 2 parents/parents-in-law. Individual/Multi-individual: Self, Spouse/Partners, Upto 3 Dependent Children, Parents & parents-in-law, Grandparents, Grandchildren, Siblings (Sister/Brother), Uncle, Aunt, Nephew, Niece, Employee, Domestic Help and Legal Guardian |
**Proportionate deduction of Associated Medical Expenses applicable in case insured person is admitted in a room whose category is higher than the eligible room category.
Disclaimer:
This is only a summary of the product features. The actual benefits available are as described in the policy, and will be subject to the policy terms, conditions, waiting periods and exclusions. Please seek the advice of your insurance advisor if you require any further information or clarification.
“Insurance is a subject matter of solicitation”. For more details on benefits, exclusions, limitations,
terms & conditions, please refer sales brochure/ policy wordings carefully, before concluding a sale.” Commencement of risk cover under the policy is subject to receipt of premium by Tata AIG General Insurance Company Limited
General Note: Exclusion are with detailed bifurgation, only 1 or 2 are extra exclusion they also immaterial no no to recheck again and again.